Bariatric Surgeons are the Latest to Get a (Mechanical) Hand in the OR
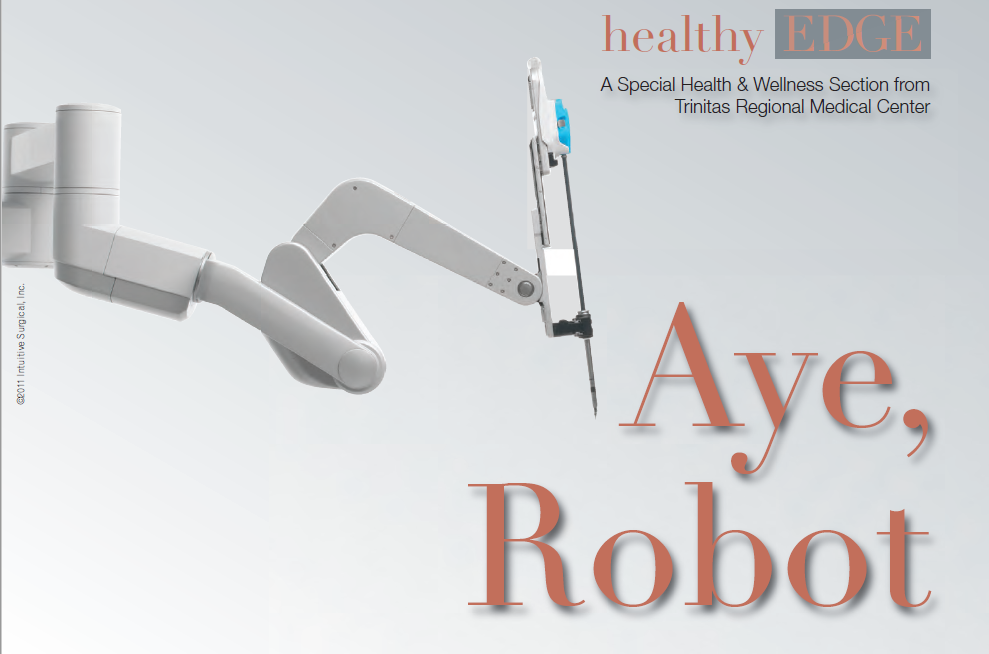
To the layperson, the melding of humans and machines sometimes seems like the stuff of science fiction. For Trinitas surgeons working with the da Vinci Surgical System, it’s just another day at the office. Now Trinitas can claim the NY Metro area’s first Robotic Bariatric Surgery program. “This program establishes Trinitas as a Center of Excellence for Robotic Surgery,” says Gary S. Horan, President/CEO of Trinitas Regional Medical Center. “It will draw patients from all over the region, as well as many from outside the region. Trinitas also becomes the place where bariatric surgeons will come to do their training.”

Who benefits from robotic bariatric surgery? Both surgeon and patient. According to Dr. Forrester, robotic bariatric surgery may open the path to good  health to patients who in the past might have been rejected as a bariatric surgical candidate. Higher-weight patients are more challenging to operate on because their body structure places limitations on conventional laparoscopic instruments. The da Vinci diminishes the problem by giving the surgeon greater control and maneuverability. The da Vinci is also good for revisional surgeries, where a bariatric patient needs a procedure redone, or must switch from a band to a bypass. Where will robotics take bariatric surgeons in the future? Anywhere they want. Indeed, seated inside the da Vinci pod and controlling the camera, a surgeon at Trinitas could theoretically perform a bypass on anyone, anywhere. This could have interesting implications for remote parts of our own country, where obesity is epidemic and trained surgeons are few.
health to patients who in the past might have been rejected as a bariatric surgical candidate. Higher-weight patients are more challenging to operate on because their body structure places limitations on conventional laparoscopic instruments. The da Vinci diminishes the problem by giving the surgeon greater control and maneuverability. The da Vinci is also good for revisional surgeries, where a bariatric patient needs a procedure redone, or must switch from a band to a bypass. Where will robotics take bariatric surgeons in the future? Anywhere they want. Indeed, seated inside the da Vinci pod and controlling the camera, a surgeon at Trinitas could theoretically perform a bypass on anyone, anywhere. This could have interesting implications for remote parts of our own country, where obesity is epidemic and trained surgeons are few.
The da Vinci system that is utilized for bariatric procedures is already on-site. It’s the techniques and training that are new to Trinitas. A team of surgeons from the hospital has completed the rigorous training involved in mastering the da Vinci robot, which is already used for minimally invasive surgeries in a number of specialties. For some of its training, the team had to fly to Maine. Of the three types of bariatric surgeries—gastric bypass, sleeve gastrectomy and gastric banding—that can be performed robotically, the bypass lends itself especially well to the da Vinci system, explains Glenn Forrester, MD, FACS, Director of Bariatric Surgery at Trinitas. The bypass requires the most fine suturing and the da Vinci allows for the exact placement of the sutures, he says. “Another significant advantage,” adds Dr. Forrester, “is that the surgeon controls the camera throughout the operation.  During a normal laparoscopic procedure, an assistant handles the camera. This gives surgeons more control over where their eyes are trained. Imagine wanting to look at something and having someone else controlling your eyes.” In a robotic procedure, the surgeon is removed from the side of the operating table. The standard operating team is around the patient. Above the patient cart is the robotic arm. There is one surgical assistant on hand to perform tasks like retracting and stapling.
During a normal laparoscopic procedure, an assistant handles the camera. This gives surgeons more control over where their eyes are trained. Imagine wanting to look at something and having someone else controlling your eyes.” In a robotic procedure, the surgeon is removed from the side of the operating table. The standard operating team is around the patient. Above the patient cart is the robotic arm. There is one surgical assistant on hand to perform tasks like retracting and stapling.
The surgeon operates remotely — with fingers manipulating ultra-responsive individual controls and feet working pedals that focus the camera and control energy to the devices. The surgeon views the procedure through a high-definition 3-D monitor. To perform robotic bariatric procedures, surgeons must receive training from da Vinci and training from Trinitas. It typically requires four days of training and observing procedures, and between 5 and 15 supervised procedures before a surgeon gets the green light to fly solo. On top of that, additional annual training is required, as the procedures and technology evolve. Is there a fear factor among patients when they hear that a robot will have a hand in the surgery? “Patients understand that it’s not a robot doing the surgery,” Dr. Forrester smiles. “The surgery is robotic-assisted. The da Vinci is only a tool.” Soon, he says, this will be viewed as just another instrument in the operating room. “Robotic bariatric procedures are safe and effective without altering the outcomes.” Any trepidation on the part of bariatric surgeons? “No,” says Dr. Forrester. “Surgeons have a technological side and the da Vinci lets us take our ability to help patients to a whole new level.”
Trinitas Is First in New Jersey to Offer New Image-Guided Breast Cancer Technology
 The term “guesswork” is not a particularly comforting one for early-stage breast cancer patients. Once a lumpectomy has been performed, the diagnosis confirmed and radiotherapy initiated, women want to know that radiation is going to the right place. Now they can check the doctor’s work for themselves. In June, Trinitas Regional Medical Center became the first cancer treatment facility in the state to offer breast cancer patients a radiotherapy technology called AccuBoost. Developed by Nucletron, a company headquartered in the Netherlands, AccuBoost enables doctors and patients to actually see the area receiving radiation treatment as it receives it. In other words, no guesswork. The system images the site where cancer was removed so that the surrounding breast tissue can be treated more accurately with boost-dose targeting. “AccuBoost utilizes real-time mammography to localize the treatment,” says Clarissa Henson, MD, Chair of Radiation Oncology at Trinitas (above). “This technology is far superior to the current standard of care treatment. On average, only 51 percent of the treatment area receives 90 percent of the dose when using the current standard of care. With AccuBoost, targeting is improved and a more effective dose of radiation is delivered to the tumor site.” With AccuBoost, a technician can position the applicator so that it delivers the therapeutic dose accurately and reliably, with limited radiation exposure to the skin. The dose is uniform over the portion of the breast that is being irradiated, which reduces unnecessary exposure of healthy tissue to radiation and enables patients to retain more undamaged tissue.
The term “guesswork” is not a particularly comforting one for early-stage breast cancer patients. Once a lumpectomy has been performed, the diagnosis confirmed and radiotherapy initiated, women want to know that radiation is going to the right place. Now they can check the doctor’s work for themselves. In June, Trinitas Regional Medical Center became the first cancer treatment facility in the state to offer breast cancer patients a radiotherapy technology called AccuBoost. Developed by Nucletron, a company headquartered in the Netherlands, AccuBoost enables doctors and patients to actually see the area receiving radiation treatment as it receives it. In other words, no guesswork. The system images the site where cancer was removed so that the surrounding breast tissue can be treated more accurately with boost-dose targeting. “AccuBoost utilizes real-time mammography to localize the treatment,” says Clarissa Henson, MD, Chair of Radiation Oncology at Trinitas (above). “This technology is far superior to the current standard of care treatment. On average, only 51 percent of the treatment area receives 90 percent of the dose when using the current standard of care. With AccuBoost, targeting is improved and a more effective dose of radiation is delivered to the tumor site.” With AccuBoost, a technician can position the applicator so that it delivers the therapeutic dose accurately and reliably, with limited radiation exposure to the skin. The dose is uniform over the portion of the breast that is being irradiated, which reduces unnecessary exposure of healthy tissue to radiation and enables patients to retain more undamaged tissue.
“The diagnosis of breast cancer is one of the mo st traumatic for any woman,” says Dr. Henson. “Being able to see treatment as it is delivered through this new technology helps patients be informed and involved in their care.” “Trinitas was the first cancer treatment center in New Jersey to offer Rapid Arc radiotherapy technology and now we are the first with AccuBoost,” adds TRMC President and CEO Gary S. Horan (right). “It’s another clear example of why Trinitas Comprehensive Cancer Center is a regional leader in cancer care.”
st traumatic for any woman,” says Dr. Henson. “Being able to see treatment as it is delivered through this new technology helps patients be informed and involved in their care.” “Trinitas was the first cancer treatment center in New Jersey to offer Rapid Arc radiotherapy technology and now we are the first with AccuBoost,” adds TRMC President and CEO Gary S. Horan (right). “It’s another clear example of why Trinitas Comprehensive Cancer Center is a regional leader in cancer care.”

Photo credit: iStockphoto/Thinkstock
Well, and limit your exposure to toxins like cigarettes and alcohol. But maintaining mental fitness is often off our radar. We go to medical doctors for checkups and tests, but we’re often reluctant to make time to review and change elements in our lives to maintain our mental health. “The mind is a miraculous and delicate thing,” says Rodger Goddard, Ph.D., chief psychologist at Trinitas Regional Medical Center. “It needs our care, protection and nurturance to continue growing throughout our lives.” Fortunately, preserving and enhancing your mental health requires only a few key lifestyle changes and simple strategies. At the top of the list? Managing stress. Stress causes surges in hormones that can damage your body— and your mind. “Stress increases the cortisol level in our brains, causing the destruction of neurons,” says Patricia Neary-Ludmer, Ph.D., a psychologist and director of Trinitas Regional Medical Center’s Family Resource Center in Cranford.
The fight-or-flight surge of adrenaline that occurs when you’re stressed can cause other damage to your brain, too. “When the lower reptilian brain is aroused by excessive stress or anger, higher brain functions tend to decrease or shut down,” Goddard points out. “Stress, anxiety and depression have been shown to decrease intelligence and cognitive skills.” There are a number of lifestyle tweaks that can improve mental acuity and fight off stress, depression and other mental-health issues. Here are some of the most effective:
Eat Smart You already know a healthy diet is essential for improving your overall physical health—but eating the right foods can improve your mental health, too. Fatty foods, especially those with saturated fats, can clog arteries and inhibit blood flow to your brain, explains Neary-Ludmer. To boost your brainpower, “eat foods like fish and nuts, which are commonly referred to as brain foods.” To further boost your brainpower, consider supplementing your diet with antioxidants and vitamins. “Studies show that diets rich in antioxidants—vitamins C, E, B and beta carotene—can help us to maintain good memory and thinking skills,” Goddard says.
Challenge Your Brain Just as your body needs regular strength and cardio training to keep it in optimal shape, your brain needs a good workout to preserve its prowess. Puzzles, animated discussions and memorization exercises can help improve your mental acuity. Goddard suggests asking yourself questions to strengthen your mind. “In particular trying to discover the causes of events and asking ourselves ‘why’ questions can strengthen our mental muscle.” Neary-Ludmer recommends challenging your brain by learning a new language, or even simply trying to write with your non-dominant hand. The payoff in mental prowess will be rich. “The more we exercise our brain and keep it active, the sharper our minds will be,” Goddard says. “Mental dullness and passivity can erode mental sharpness.”

Photo credit: iStockphoto/Thinkstock
Get a Good Workout Exercise isn’t just good for building muscles—it helps build mental acuity, too. “Exercise will increase blood flow to the brain, carrying oxygen and nutrients,” Neary-Ludmer says. A good workout plays a key role in ensuring good mental health. “Physical exercise has been shown to increase brain chemicals that improve memory, reaction speed and creativity,” Goddard adds.
Meditate You don’t have to do a full-on “just say ohm” yoga retreat—but taking a few minutes each day to clear your mind, breathe deeply and relax can have benefits beyond simple stress relief. “Meditation has been shown to increase mental focus, awareness and some thinking skills,” Goddard says.
See the Glass as Half Full Look for ways to increase the amount of fun in your life—whether it’s listening to upbeat music, limiting the amount of time you spend with negative people, or adjusting your own attitude to accentuate the positive. “Studies have shown that thinking positive, loving and caring thoughts can improve neural connections in the brain,” Goddard says.
Get a Good Night’s Sleep You’ve likely heard (and heard again) that a good night’s sleep—about eight hours a night—is essential for good physical health. But it’s also important for keeping your brain at peak performance. “Good sleep habits have been shown to improve brain functioning and mental agility,” Goddard says. Do your best to ensure you get the right amount of rest every night.

Photo credit: iStockphoto/Thinkstock
Be Wary of Multi-tasking It may feel like your brain’s firing on all cylinders—and that you’re accomplishing more—by multi-tasking, but the jury’s still out as to whether multitasking is harmful or helpful to your mental health. “It is still unclear whether the multi-tasking demands of our modern world enhance or deteriorate mental sharpness,” Goddard says. “At least for some people, excessive multi-tasking may lead to being more scattered, unfocused and having decreased concentration and memorization skills.” If it seems like your ability to focus has diminished, consider trying to limit the amount of multi-tasking you do.
Break Out of Your Routine “It is easy for all of us to fall into ruts and experience our stress and problems as unchangeable,” Goddard says. But thinking outside the box—and moving outside your comfort zone—gives your brain the kind of kick-start you need to stay sharp. “Traveling, journaling and using personal or spiritual retreats can help us to reflect on our lives and chart new goals.” A quick getaway or a new class can be all you need to break out of the rut—and get on the road to a sharper mind. EDGE
Editor’s Note: Lisa Milbrand is a New Jersey-based writer whose articles on health and relationships appear in Parents, Arthritis Today and Modern Bride. Her blog themamahood.com celebrates the life of a working mother.
 Pancreatic Cancer May Not Be A Death Sentence When we hear the words Pancreatic Cancer we shudder. And rightfully so. By the time the first symptoms develop—unexplained abdominal pain, weight loss, poor appetite, jaundice—and the tumor is picked up by a CT scan or MRI, the disease is uniformly fatal. According to Dr. Dan Ramasamy, a gastroenterologist at the Center for Digestive Diseases in Union, Pancreatic Cancer actually can be cured—when caught in its earliest stages. Early stage diagnosis is accomplished through Endoscopic Ultrasound (EUS). A special ultrasound device installed on the tip of the endoscope enables examination from the stomach through to the pancreas. With EUS, the pancreas can be visualized with high-quality ultrasound images, detecting tumors as small as a few millimeters, which can be missed by a CT Scan or MRI. According to Dr. Ramasamy, who performs this procedure, a biopsy can be taken through the stomach wall with fine needle aspiration (FNA) and sent for evaluation. If still in its earliest stage, the cancer is curable by surgery.
Pancreatic Cancer May Not Be A Death Sentence When we hear the words Pancreatic Cancer we shudder. And rightfully so. By the time the first symptoms develop—unexplained abdominal pain, weight loss, poor appetite, jaundice—and the tumor is picked up by a CT scan or MRI, the disease is uniformly fatal. According to Dr. Dan Ramasamy, a gastroenterologist at the Center for Digestive Diseases in Union, Pancreatic Cancer actually can be cured—when caught in its earliest stages. Early stage diagnosis is accomplished through Endoscopic Ultrasound (EUS). A special ultrasound device installed on the tip of the endoscope enables examination from the stomach through to the pancreas. With EUS, the pancreas can be visualized with high-quality ultrasound images, detecting tumors as small as a few millimeters, which can be missed by a CT Scan or MRI. According to Dr. Ramasamy, who performs this procedure, a biopsy can be taken through the stomach wall with fine needle aspiration (FNA) and sent for evaluation. If still in its earliest stage, the cancer is curable by surgery.
Smart Kids & Stupid Decisions Two recent studies, one in the U.S. and one in England, reveal that “very bright” kids  are more likely than children of average intelligence to be heavy drinkers when they grow up. The studies—National Longitudinal Study of Adolescent Health (US) and National Child Development Study (UK)—took into account religion, sex, race, ethnicity, marital status, number of children, education, earnings, satisfaction with life, frequency of socialization with friends, depression, number of recent sex partners, childhood social class, mother’s education, and father’s education—and still came up with the same results. Satoshi Kanazawa, an evolutionary psychologist and author of Why Beautiful People Have More Daughters, offered one interesting theory for this phenomenon. Intelligent people aremore likely to be “early adopters,” so it makes sense they would adopt beer, wine and distilled spirits—which are acquired tastes as opposed to evolutionary staples.
are more likely than children of average intelligence to be heavy drinkers when they grow up. The studies—National Longitudinal Study of Adolescent Health (US) and National Child Development Study (UK)—took into account religion, sex, race, ethnicity, marital status, number of children, education, earnings, satisfaction with life, frequency of socialization with friends, depression, number of recent sex partners, childhood social class, mother’s education, and father’s education—and still came up with the same results. Satoshi Kanazawa, an evolutionary psychologist and author of Why Beautiful People Have More Daughters, offered one interesting theory for this phenomenon. Intelligent people aremore likely to be “early adopters,” so it makes sense they would adopt beer, wine and distilled spirits—which are acquired tastes as opposed to evolutionary staples.
Smoking, Obesity Increase CRC Risk in Women With so much attention focused on urging men to get checked out for colorectal cancer (CRC), people sometimes forget that this is the third most common cause of cancer in women. Adding to the threat is the fact that screening guidelines are not “one-size-fits-all” for men and women. Indeed, according to a May article in Women’s Health, myriad factors contribute to determining the right screening intervals for female patients. The article also cited recent studies that have shown smoking and obesity increase the risk of CRC in women. Screening for CRC increases the chances for early detection of cancer and premalignant polyps, and also decreases morbidity from this disease.
 Stamping Out Alzheimer’s The effort to understand, treat and perhaps ultimately prevent Alzheimer’s Disease depends on raising funds and awareness. In May, these goals got some help from Maryland Senator Barbara Mikulski, who introduced a resolution in the House of Representatives urging the U.S. Postal Service to issue a special stamp to help raise money for Alzheimer’s research. Mikulski’s own father was one of an estimated 5.4million Americans diagnosed with the disease. By voluntarily paying more than the normal postage rate for the Alzheimer’s stamp, people would contribute directly to the search for a new treatment or a cure.
Stamping Out Alzheimer’s The effort to understand, treat and perhaps ultimately prevent Alzheimer’s Disease depends on raising funds and awareness. In May, these goals got some help from Maryland Senator Barbara Mikulski, who introduced a resolution in the House of Representatives urging the U.S. Postal Service to issue a special stamp to help raise money for Alzheimer’s research. Mikulski’s own father was one of an estimated 5.4million Americans diagnosed with the disease. By voluntarily paying more than the normal postage rate for the Alzheimer’s stamp, people would contribute directly to the search for a new treatment or a cure.
The fast-food Drive-Thru has transformed our lives. Well, that’s one way of looking at it.
Fast food giant Taco Bell recently became embroiled in a high-profile lawsuit, during which it was compelled to respond to allegations that its “beef filling”
contained— what’s the delicate way of putting this? —twice as much “filling” as “beef.” The media seized on this story, as did the late-night comics. Unfortunately, everyone missed the point: The crime is what’s in fast food, not what isn’t. “Fast food poses a huge threat to the American public’s health, along with smoking and substance abuse,” says Ari Eckman, MD, chief of the Division of Endocrinology, Diabetes & Metabolism and director of The Diabetes Management Center at Trinitas Regional Medical Center. “Fast food meals are high in fat, sugar, salt, starch and calories, and very low in fiber and nutrients.” Indeed, the convenience of grab-and-go meals is far outweighed by the dangers that await us after we make that final hard left to the pickup window. Study after study is showing that reliance on heavily processed foods could be costing us our health. In a 2005 report published in The Lancet, healthy young adults who consumed fast food more than twice each week gained 10 more pounds and had twice as great an increase in insulin resistance—a precursor to type-2 diabetes—as their healthier eating counterparts. Fast foods are rich in trans fats, those manmade fats that have been shown to wreak havoc on the human heart. “Trans fats are terrible for one’s cholesterol,” Dr. Eckman says. “It’s dangerous to eat these foods if you have high blood pressure
e or high cholesterol.” Fast food isn’t just a nutritional nightmare. With the constant push to supersize, fast food portions are warping our sense of when to say when. “People are not at all in touch with the reality of how much they’re eating,” Dr. Eckman says. “The portion sizes are encouraging people to eat more. Burgers 50 years ago were only one ounce, and now they’re six ounces. You buy a 64-ounce soda, which is a half-gallon— and contains 48 teaspoons of sugar.” As a result, Dr. Eckman maintains, our society is becoming supersized. “Over 60 percent of our population is overweight, and 30 percent is obese,” he says. “And the children’s statistics are even more mind-boggling—nine million American kids were considered obese, a rate that has nearly doubled in the last 20 years. It’s getting out of control at an epidemic rate.” Fortunately, there are measures you can take to fight back—even if you have to eat fast:
overweight, and 30 percent is obese,” he says. “And the children’s statistics are even more mind-boggling—nine million American kids were considered obese, a rate that has nearly doubled in the last 20 years. It’s getting out of control at an epidemic rate.” Fortunately, there are measures you can take to fight back—even if you have to eat fast:
- Check the labels. Most fast-food restaurants offer nutritional information on their websites or on pamphlets, which enables you to make a more informed decision about what you order. “Try to stay away from the foods that are highest in cholesterol, saturated fats, sugar and salt,” Dr. Eckman says. “Choose low-fat options, if they’re available.” Keep in mind that that healthy salad may come with a not so – healthy dressing, so resist the temptation to squeeze the entire packet onto your greens.
- Cut down on your portions. Avoid the push to supersize your meal—those value menus may be a better deal
 financially, but could cost you your health. “To help spread out the calories, consider eating half of it and giving the other half to your partner or taking it home for another meal,” Dr. Eckman advises.
financially, but could cost you your health. “To help spread out the calories, consider eating half of it and giving the other half to your partner or taking it home for another meal,” Dr. Eckman advises. - Turn your kids into educated eaters. The fast-food commercials—and those little plastic toys—may entice your kids into clamoring for a drive-thru run, but you can fight back. “Making a healthy dinner at home can be a fun activity you do with your kids, that can help encourage them to eat healthier,” Dr. Eckman suggests. “You can also talk with your kids about the problem of obesity and some of its long-term effects on health, so they can become educated and make healthier choices on their own.”
- Moderation. Dr. Eckman suggests limiting fast food to only one meal per week, at the most. “Enjoy it once in a while, but this really shouldn’t be a weekly or biweekly event,” he says. “You don’t want to sacrifice your health for convenience.” EDGE
Editor’s Note: Lisa Milbrand is a New Jersey-based writer whose articles on health and relationships appear in Parents, Arthritis Today and Modern Bride. Her blog themamahood.com celebrates the life of a working mother.

Cold feet. Heavy legs. Cramping. As the years pile up, we deal with life’s extra little discomforts every day. They can be a real pain in the you-know what. Dealing with them, however, does not mean ignoring them. If annoyances such as these persist, it may be prudent to speak with a vascular surgeon. The fact of the matter is that each of the aforementioned symptoms (including, yes, buttock pain) could point to something more serious. “We’re not talking about spider veins here,” says Salvador Cuadra, MD. “Vascular system disorders such as Peripheral Artery Disease (PAD) and Carotid Artery Disease—including Transient Ischemic Attacks (TIAs)—can begin with relatively mild symptoms. The earlier we catch these problems, the more likely a patient is going to have a favorable outcome.” As a vascular  surgeon, Dr. Cuadra is a specialist who treats diseases of the major blood vessels. A member of the Cardiovascular Care Group (with offices at Trinitas and in Westfield, Springfield and Belleville), he treats problems with the carotid arteries in the neck, as well as the veins and arteries in the abdomen, arms and lower extremities. One of Dr. Cuadra’s specialties is called a carotid endarterectomy. In lay terms, this is a surgical procedure that addresses blockages in the artery feeding the brain. Plaque can build up and potentially cause a stroke. The surgery literally “shells out,” or removes, the plaque through a small neck incision. Although the condition is extremely serious, the surgical prognosis is excellent and recovery time is relatively short. Typically, it involves only an overnight hospital stay. Within the past decade, there have been other advances in the development of less invasive treatments for vascular system disorders. Most of these involve the use of stents, which are applied through a catheter inserted through the groin area. The less invasive nature of this procedure certainly makes it more attractive to patients. Vascular surgeons routinely perform angioplasty to repair arteries that are blocked or narrowed. There has been much recent research and discussion about the relative efficacy of stents compared to surgery. The much-publicized CREST Trial has indicated that stents have no statistical advantage over surgery and, in certain cases, might even run a higher risk of subsequent stroke. However, Dr. Cuadra is uniquely qualified to perform either angioplasty or surgery. He has found that some patients have better results with angioplasty and stents, while others benefit more from surgery. Another problem that can be addressed by inserting a stent is an aneurysm. In such a case, an artery develops a bulge (widening) rather than a blockage. Over time, this can cause a weakening in the arterial wall. A vascular surgeon will perform a procedure to insert a specialized stent that allows blood to pass through it removing the pressure on the arterial wall (the aneurysm) thereby reducing the risk of rupture. At present, dialysis patients constitute approximately 50% of Dr. Cuadra’s group practice. In cases of kidney failure— which requires hemodialysis to remove toxic waste and excess fluid from the bloodstream—surgery is done to establish the necessary connection between an artery and a vein thereby allowing for dialysis to be performed. Of the remaining 50%, different people land in his office in a number of different ways. Many patients come via their PCP referral already suffering from obesity and/or diabetes; their doctor may have found an abnormality through physical examination or through an ultrasound, or some other procedure such as a CT scan. Others come because of physical symptoms such as loss of circulation to the legs causing pain, ulcerations, and even gangrene in the extremity. Although Dr. Cuadra says he enjoys working with patients to prevent the onset of vascular disease, he embraces the myriad challenges he faces every day. Being a surgeon suits him, he says. “I like using my hands to solve relatively serious patient problems. Surgery is more rewarding to me than some other specialties. I can see a problem, diagnose it and fix it in a relatively short time period.” EDGE
surgeon, Dr. Cuadra is a specialist who treats diseases of the major blood vessels. A member of the Cardiovascular Care Group (with offices at Trinitas and in Westfield, Springfield and Belleville), he treats problems with the carotid arteries in the neck, as well as the veins and arteries in the abdomen, arms and lower extremities. One of Dr. Cuadra’s specialties is called a carotid endarterectomy. In lay terms, this is a surgical procedure that addresses blockages in the artery feeding the brain. Plaque can build up and potentially cause a stroke. The surgery literally “shells out,” or removes, the plaque through a small neck incision. Although the condition is extremely serious, the surgical prognosis is excellent and recovery time is relatively short. Typically, it involves only an overnight hospital stay. Within the past decade, there have been other advances in the development of less invasive treatments for vascular system disorders. Most of these involve the use of stents, which are applied through a catheter inserted through the groin area. The less invasive nature of this procedure certainly makes it more attractive to patients. Vascular surgeons routinely perform angioplasty to repair arteries that are blocked or narrowed. There has been much recent research and discussion about the relative efficacy of stents compared to surgery. The much-publicized CREST Trial has indicated that stents have no statistical advantage over surgery and, in certain cases, might even run a higher risk of subsequent stroke. However, Dr. Cuadra is uniquely qualified to perform either angioplasty or surgery. He has found that some patients have better results with angioplasty and stents, while others benefit more from surgery. Another problem that can be addressed by inserting a stent is an aneurysm. In such a case, an artery develops a bulge (widening) rather than a blockage. Over time, this can cause a weakening in the arterial wall. A vascular surgeon will perform a procedure to insert a specialized stent that allows blood to pass through it removing the pressure on the arterial wall (the aneurysm) thereby reducing the risk of rupture. At present, dialysis patients constitute approximately 50% of Dr. Cuadra’s group practice. In cases of kidney failure— which requires hemodialysis to remove toxic waste and excess fluid from the bloodstream—surgery is done to establish the necessary connection between an artery and a vein thereby allowing for dialysis to be performed. Of the remaining 50%, different people land in his office in a number of different ways. Many patients come via their PCP referral already suffering from obesity and/or diabetes; their doctor may have found an abnormality through physical examination or through an ultrasound, or some other procedure such as a CT scan. Others come because of physical symptoms such as loss of circulation to the legs causing pain, ulcerations, and even gangrene in the extremity. Although Dr. Cuadra says he enjoys working with patients to prevent the onset of vascular disease, he embraces the myriad challenges he faces every day. Being a surgeon suits him, he says. “I like using my hands to solve relatively serious patient problems. Surgery is more rewarding to me than some other specialties. I can see a problem, diagnose it and fix it in a relatively short time period.” EDGE
Editor’s Note: Dr. Salvador Cuadra attended Cornell University as an undergrad and received his medical degree—and became Chief Resident in surgery—at the State University of New York at Stony Brook. He has authored a number of vascular surgery treatises, receiving awards for several of his publications.
Why resolutions fail (and how yours can succeed).
 If you’re planning to make 2011 the year you lose weight and get fit, join the club: Studies show these are the most common resolutions people make come January 1st. Good luck to you; the grim reality is that most of the people who start the year off wanting to slim down don’t end up succeeding. The same goes for other popular New Year’s vows—stop smoking, get out of debt, help others, etc., etc. etc. The bottom line is that we just aren’t wired to break habits overnight that we’ve developed over 10, 20 or 30 years. As individuals, human beings tend to value their individuality. As a species, we’re just plain stubborn. Some great minds have weighed in on this subject. The controversial author Anaïs Nin insisted she made no resolutions to curb her habits, because “the habit of making plans, of criticizing, sanctioning and molding my life, is too much of a daily event for me.” Sculptor Henry Moore preferred to “think in terms of the day’s resolutions, not the year’s.” Writer Oscar Wilde, whose list of questionable habits was practically endless, characterized resolutions as “checks that men draw on a bank where they have no account.” Comic Joey Adams’s favorite party toast was “May all your troubles last as long as your New Year’s resolutions.” Mark Twain evaluated New Year’s resolutions with a single word: Humbug. Given this overwhelming preponderance of intellectual evidence, what chance do we mere mortals have to drop a few pounds and elevate our fitness? According to Michelle Ali, a registered dietician at Trinitas Regional Medical Center, there are 10 things we can do to improve the odds:
If you’re planning to make 2011 the year you lose weight and get fit, join the club: Studies show these are the most common resolutions people make come January 1st. Good luck to you; the grim reality is that most of the people who start the year off wanting to slim down don’t end up succeeding. The same goes for other popular New Year’s vows—stop smoking, get out of debt, help others, etc., etc. etc. The bottom line is that we just aren’t wired to break habits overnight that we’ve developed over 10, 20 or 30 years. As individuals, human beings tend to value their individuality. As a species, we’re just plain stubborn. Some great minds have weighed in on this subject. The controversial author Anaïs Nin insisted she made no resolutions to curb her habits, because “the habit of making plans, of criticizing, sanctioning and molding my life, is too much of a daily event for me.” Sculptor Henry Moore preferred to “think in terms of the day’s resolutions, not the year’s.” Writer Oscar Wilde, whose list of questionable habits was practically endless, characterized resolutions as “checks that men draw on a bank where they have no account.” Comic Joey Adams’s favorite party toast was “May all your troubles last as long as your New Year’s resolutions.” Mark Twain evaluated New Year’s resolutions with a single word: Humbug. Given this overwhelming preponderance of intellectual evidence, what chance do we mere mortals have to drop a few pounds and elevate our fitness? According to Michelle Ali, a registered dietician at Trinitas Regional Medical Center, there are 10 things we can do to improve the odds: 
1 Don’t Go Overboard There’s a real temptation to sprint out of the gate and make drastic changes to your diet and workout routines. But being gung-ho from the get-go can lead to burnout and failure down the line. “Unrealistic goals hurt us more than we realize,” says Ali. “Weight loss should be slow, about a pound a week.” She advises skipping a full-scale renovation in favor of making slow and subtle changes that can become a permanent part of your life. “Make one food change each month and stick to it. That’ll make weight loss happen—and make it permanent.”
2 Monitor Portion Size Those supersized portions of food you often see at restaurants are rarely the right amount of food to keep you at a healthy size. “Far too often we are unaware of what a serving of a particular food is,” Ali says. “For example, for protein foods such as chicken or beef, a serving is considered to be 3 ounces, or the size of a deck of cards. Most Americans consumes more than twice the amount of protein that is needed by their bodies.”
3 Don’t Skip Meals It may seem like a smart idea to avoid eating those extra calories, but studies show that this method can backfire, especially if it’s breakfast that you skip. “Breakfast really sets the mood for the rest of the day,” Ali says. “Skipping breakfast slows down your metabolism and causes you to overeat at other times.”
4 Create a Food Diary Keep track of what you’re eating and when. Studies have shown that writing down your daily diet can help you consume fewer calories and be more thoughtful about the choices you make. If you don’t want to use a pad of paper, consider signing up for an online weight-loss tool like SparkPeople.com, where you can record your daily diet and track calories, protein, fat and more.
5 Be Salad Savvy You may feel very virtuous with that plate of greens in front of you, but the dreamy dressing you choose could turn that salad into a caloric nightmare. “One frequent mistake that people make is that they load up on salads and use far too much salad dressing,” Ali says. “Regular salad dressings are loaded with calories, which comes mainly from fat and, when use in abundance, defeat the purpose.” Stick with vinaigrettes in lieu of the creamier mayonnaise-based dressings, or make a simple (and delicious) one at home with olive oil, lemon juice and vinegar.
6 Read the Label You might be surprised to find that that can of soup or container of ice cream that claims to be healthier for you actually comes with a pretty hefty calorie count. “You will be surprised at what you’ll find when you compare one product to another—especially when we compare things like fat, sugar and sodium,” Ali says. “Be sure to look at some dietetic foods that may claim to be low in sugar and or fat—you may find that the regular product is lower in total calories.”
7 Avoid Fad Diets There’s always a new trendy diet to try—high-protein, low-carb, no-fat, the infamous cabbage soup diet—but even if you start off your fad diet peeling off the pounds, odds are the effects won’t last. “Crash diets never lead to permanent weight loss,” Ali says. “To succeed, you must commit to a healthy lifestyle for a lifetime.”
8 Exercise Cutting back on your food intake is only one piece of the puzzle. For consistent weight loss success, you’re going to have to work up a sweat. “When we lose weight we lose both fat and muscle, but exercise can preserve lean body mass,” Ali says. “Exercise speeds up our metabolism and helps us to burn more calories—and toned muscles also make us look better in our clothes.”
9 Make It Fun “If jogging’s not your thing, find an activity you enjoy doing,” Ali says. That way, exercise doesn’t become a chore—it’s an enjoyable part of your day.
10 Don’t Give Up Even if you had a bad day (and a Snickers bar or two), it isn’t the end of the world—or even the end of your diet. Remember that tomorrow is another day. Vow to do better. EDGE
Feel like strangling Santa? You’re not alone. And there’s probably nothing wrong with you, either.
Tradition tells us that this time of year is meant for “Decking the Halls.” But did you ever feel like decking a friend or family member instead? All kidding aside,  the mini-bouts of depression and anger that sometimes accompany this season are very real. The holiday blues can grip even the happiest, most well-adjusted of us with little or no warning. Understanding where these feelings come from, as well as your options for addressing them, can go a long way toward making it to January with your sanity intact. According to Dr. Rodger Goddard, who has served as Chief Psychologist at Trinitas Regional Medical Center for more than two decades, stress is almost always the trigger. And holiday stress can come from many sources. “At the end of the year, during the holidays, we reflect on our lives,” he explains. “When we reflect, we can get nervous about many things. For instance, many of us now face intense financial stress due to the state of the economy. This kind of reflection often leads us to dwell on our shortcomings and what we don’t have, rather than our accomplishments and the miracle of just being alive.” Dealing with relatives can just compound the situation. Tension between different family members, dwelling on past hurts or injustices, rivalries and jealousies can bring old wounds back to the surface. In this environment, little things—such as where to eat, what to eat and who sits where—can become incredibly stressful and suck the joy out of what should be pleasant reconnections and reunions. “On top of this,” Dr. Goddard adds, “we often eat and drink too much. The result is body discomfort, which contributes to distressing emotions.” The media can play a leading role in feelings of depression and anger. Movies, music, television shows and commercials all make the holidays out to be a magical time of happiness and perfection. To feel otherwise just feels wrong. “We live in reality, not a movie,” says Dr. Goddard. “Holidays cramp our schedule—overloading us with shopping, socializing, preparations and party-going. The holiday season has become hyper-commercialized, giving us the message that love is shown through material gift-giving. Under these conditions, we can feel that what we give and what we get are being constantly evaluated—which leads to even more stress.”
the mini-bouts of depression and anger that sometimes accompany this season are very real. The holiday blues can grip even the happiest, most well-adjusted of us with little or no warning. Understanding where these feelings come from, as well as your options for addressing them, can go a long way toward making it to January with your sanity intact. According to Dr. Rodger Goddard, who has served as Chief Psychologist at Trinitas Regional Medical Center for more than two decades, stress is almost always the trigger. And holiday stress can come from many sources. “At the end of the year, during the holidays, we reflect on our lives,” he explains. “When we reflect, we can get nervous about many things. For instance, many of us now face intense financial stress due to the state of the economy. This kind of reflection often leads us to dwell on our shortcomings and what we don’t have, rather than our accomplishments and the miracle of just being alive.” Dealing with relatives can just compound the situation. Tension between different family members, dwelling on past hurts or injustices, rivalries and jealousies can bring old wounds back to the surface. In this environment, little things—such as where to eat, what to eat and who sits where—can become incredibly stressful and suck the joy out of what should be pleasant reconnections and reunions. “On top of this,” Dr. Goddard adds, “we often eat and drink too much. The result is body discomfort, which contributes to distressing emotions.” The media can play a leading role in feelings of depression and anger. Movies, music, television shows and commercials all make the holidays out to be a magical time of happiness and perfection. To feel otherwise just feels wrong. “We live in reality, not a movie,” says Dr. Goddard. “Holidays cramp our schedule—overloading us with shopping, socializing, preparations and party-going. The holiday season has become hyper-commercialized, giving us the message that love is shown through material gift-giving. Under these conditions, we can feel that what we give and what we get are being constantly evaluated—which leads to even more stress.”
Mind-Heart-Body-Soul So what’s a seasonal sour-puss to do? Creating a “radical support” plan for the holidays should alleviate a good deal of the stress.  According to Dr. Goddard, your anti-stress strategy should look something like this:
According to Dr. Goddard, your anti-stress strategy should look something like this:
MIND — Make a PIPS list (Problem Identification/Problem Solving); for each thing that worries you about the holidays, write down a reasonable solution.
HEART — Spell out the actions that you will take to protect yourself and nurture yourself emotionally—specifically, commit to do the things that you love doing, with the people that you love the most.
BODY — Formulate a plan to limit your intake of the things that are great in moderation, but make you feel lousy in excess: sugar, starch, desserts, alcohol, cholesterol—you know, all the good stuff. Also, write down a daily workout regimen and stick to it. Exercise and movement actually processes negative emotions out of the body.
SOUL — Spell out your life mission and purpose. List the good things you have achieved during the past year. Look toward the year ahead and identify what you will do to experience a deeper spiritual feeling—anything from connecting with nature to taking a Tai Chi class. “We all try very hard to make life work,” says Dr. Goddard. “Always remember that you deserve the best.” EDGE
Editor’s Note: Dr. Goddard also directs Trinitas’s Wellness Management Services, which provides training, consultation and program development to companies and schools to improve employee, teacher and corporate health, effectiveness and success.
Nothing to Sneeze At
Dealing with dander can be a matter of life and death
Dogs may qualify as man’s best friend, but they won’t do you any favors if you’re among the estimated 10 percent of Americans who have animal-related allergies. That means your allergic antibodies—aka immunoglobulin E—have declared pet dander and saliva as enemies of the state. The casualty list in this epic, microscopic battle being waged within your body includes a runny nose, scratchy throat, watery eyes, itchy hives and, in the most serious cases, a potentially lifethreatening asthma attack. “Pet dander can activate cells in the immune system,” confirms Samuel D. Kahnowitz, MD, FCCP, FACP, Chief of Pulmonary Medicine and Medical Director of Respiratory Therapy at Trinitas Regional Medical Center. “The body then makes inflammatory substances that constrict the muscles around the airway, and cause swelling on the inside of the airways, making it harder to breathe.” Reactions to pet allergies account for an increasing number of doctor and emergency room visits in this country, so the medical community is taking this trend seriously. To a layman, at least, the obvious question is, “Has pet dander somehow gotten ‘worse’ or are people becoming more sensitive to it?” Actually the same question could be asked about our food and environment—allergies in general seem to be more prevalent, and more serious, than ever. It turns out that we may be the problem. Indeed studies suggest that our country’s obsession with cleanliness may be to blame for creating hypersensitive immune systems, which now react to harmless things around us. “Our environment has improved, so we don’t have to worry about fighting off dangerous parasites,” explains Richard J. Bukosky, MD, an allergist in Linden. “The allergic antibody doesn’t have a whole lot to do. It starts to ‘pick’ on things that we’re exposed to in the environment that are completely harmless.” While there is still no permanent cure for pet allergies, there are plenty of options available for minimizing their effects on your life—and many of them don’t require finding a new home for Fluffy or Fido: Minimize exposure to pets. The less exposure to the offending pet, the better. Opting to find a new home for your pet may help in the long run, though it can take up to 20 weeks after the pet leaves before the allergen levels really dissipate.
The casualty list in this epic, microscopic battle being waged within your body includes a runny nose, scratchy throat, watery eyes, itchy hives and, in the most serious cases, a potentially lifethreatening asthma attack. “Pet dander can activate cells in the immune system,” confirms Samuel D. Kahnowitz, MD, FCCP, FACP, Chief of Pulmonary Medicine and Medical Director of Respiratory Therapy at Trinitas Regional Medical Center. “The body then makes inflammatory substances that constrict the muscles around the airway, and cause swelling on the inside of the airways, making it harder to breathe.” Reactions to pet allergies account for an increasing number of doctor and emergency room visits in this country, so the medical community is taking this trend seriously. To a layman, at least, the obvious question is, “Has pet dander somehow gotten ‘worse’ or are people becoming more sensitive to it?” Actually the same question could be asked about our food and environment—allergies in general seem to be more prevalent, and more serious, than ever. It turns out that we may be the problem. Indeed studies suggest that our country’s obsession with cleanliness may be to blame for creating hypersensitive immune systems, which now react to harmless things around us. “Our environment has improved, so we don’t have to worry about fighting off dangerous parasites,” explains Richard J. Bukosky, MD, an allergist in Linden. “The allergic antibody doesn’t have a whole lot to do. It starts to ‘pick’ on things that we’re exposed to in the environment that are completely harmless.” While there is still no permanent cure for pet allergies, there are plenty of options available for minimizing their effects on your life—and many of them don’t require finding a new home for Fluffy or Fido: Minimize exposure to pets. The less exposure to the offending pet, the better. Opting to find a new home for your pet may help in the long run, though it can take up to 20 weeks after the pet leaves before the allergen levels really dissipate.  If your dog or cat is here to stay, make sure to keep it out of your bedroom—the place where you spend most of your time—and wash your hands thoroughly after you’ve touched your pet. Weekly bathing or grooming (done by someone other than the person with the allergies) may also help keep allergens at bay. Keep it clean. Daily vacuuming and washing-down of surfaces can help clear some of the allergens—especially if you use a vacuum with a HEPA filter that can trap the tiny particles. Removing carpeting, drapery, stuffed toys and other soft fabrics can help reduce the number of places where pet dander can become trapped. “I really push for them to allergy-proof the bedroom—get rid of the carpeting and the animals, get a dehumidifier and a HEPA filter, avoid down comforters and get allergy-proofing casing for the pillows and mattresses,” Dr. Bukosky says. Consider that it might not be your pet. Even if allergy testing turns up an allergic reaction, it may not actually be your animal that’s causing the wheezing. “Dogs roam around, and it might not be the dog himself—it may be an irritant he’s picking up outside, like wood chips or rag weed,” says Dr. Kahnowitz. Take antihistamines. Newer over-the-counter formulations, like Zyrtec and Claritin, are more potent and less likely to cause drowsiness and other unpleasant side effects. Try a more serious approach. Doctors have become more aggressive in treating allergies, often including steroids in the treatment plan. “We’re pushing steroids more,” Dr. Bukosky says. “We used to use a montelukast (Singulair) a lot, but we’ve started to use inhaled steroids more—for nasal allergies, internasal steroids are a good option.” Of course, pet allergies can also be treated with a program of allergy immunizations. “We push for immunizations, which make it less likely that you’ll develop asthma,” says Dr. Bukosky. The regimens generally start with weekly shots, then as the treatment progresses, patients can go longer and longer between injections. Finally, there’s the do-nothing approach. These are the people who claim they have built an immunity to their animal. Is this really possible? The answer is yes…and no. Dr. Bukosky warns that what these pet owners believe to be happening may not actually be the case. “With daily exposure to the pet, a person with allergies may be having mild allergy-like attacks each day that use up the IgE antibody—just not enough to cause symptoms,” he says. “Then the child goes off to college, or is away from the pet for a long vacation, and has an asthma attack. So you may become ‘used to’ your pet, but you have to be in constant contact with it to avoid a serious reaction.”
If your dog or cat is here to stay, make sure to keep it out of your bedroom—the place where you spend most of your time—and wash your hands thoroughly after you’ve touched your pet. Weekly bathing or grooming (done by someone other than the person with the allergies) may also help keep allergens at bay. Keep it clean. Daily vacuuming and washing-down of surfaces can help clear some of the allergens—especially if you use a vacuum with a HEPA filter that can trap the tiny particles. Removing carpeting, drapery, stuffed toys and other soft fabrics can help reduce the number of places where pet dander can become trapped. “I really push for them to allergy-proof the bedroom—get rid of the carpeting and the animals, get a dehumidifier and a HEPA filter, avoid down comforters and get allergy-proofing casing for the pillows and mattresses,” Dr. Bukosky says. Consider that it might not be your pet. Even if allergy testing turns up an allergic reaction, it may not actually be your animal that’s causing the wheezing. “Dogs roam around, and it might not be the dog himself—it may be an irritant he’s picking up outside, like wood chips or rag weed,” says Dr. Kahnowitz. Take antihistamines. Newer over-the-counter formulations, like Zyrtec and Claritin, are more potent and less likely to cause drowsiness and other unpleasant side effects. Try a more serious approach. Doctors have become more aggressive in treating allergies, often including steroids in the treatment plan. “We’re pushing steroids more,” Dr. Bukosky says. “We used to use a montelukast (Singulair) a lot, but we’ve started to use inhaled steroids more—for nasal allergies, internasal steroids are a good option.” Of course, pet allergies can also be treated with a program of allergy immunizations. “We push for immunizations, which make it less likely that you’ll develop asthma,” says Dr. Bukosky. The regimens generally start with weekly shots, then as the treatment progresses, patients can go longer and longer between injections. Finally, there’s the do-nothing approach. These are the people who claim they have built an immunity to their animal. Is this really possible? The answer is yes…and no. Dr. Bukosky warns that what these pet owners believe to be happening may not actually be the case. “With daily exposure to the pet, a person with allergies may be having mild allergy-like attacks each day that use up the IgE antibody—just not enough to cause symptoms,” he says. “Then the child goes off to college, or is away from the pet for a long vacation, and has an asthma attack. So you may become ‘used to’ your pet, but you have to be in constant contact with it to avoid a serious reaction.”
 Heart attack victims who have pets tend to live longer. Watching fish in a tank can lower blood pressure. In senior adults, canine companionship can keep mental health complications from turning into physical deterioration. Indeed, considerable evidence supports the healing potential of pet therapy. There is plenty of history to back up the power of pet therapy, too. The first documented account of animal therapy dates back to the 9th century in Gheel, Belgium, where farm animals were used to help disabled people cope. In Washington, D.C. in 1919, psychiatric patients at St. Elizabeth’s Hospital had dogs available for their recognized therapeutic value. And in the decades since, the medical community has come to embrace this interactive approach to improving the quality of life, both for patients in recovery and for those whose health may be in decline. For the record, today the more politically correct term for pet-related therapy is either Animal-Assisted Activities (AAA) or Animal-Assisted Therapy (AAT). AAA is a more casual meet-and-greet approach to hands-on contact between patients and pets, while AAT is a more formal clinical approach with patients who may be challenged physically, emotionally, or mentally.
Heart attack victims who have pets tend to live longer. Watching fish in a tank can lower blood pressure. In senior adults, canine companionship can keep mental health complications from turning into physical deterioration. Indeed, considerable evidence supports the healing potential of pet therapy. There is plenty of history to back up the power of pet therapy, too. The first documented account of animal therapy dates back to the 9th century in Gheel, Belgium, where farm animals were used to help disabled people cope. In Washington, D.C. in 1919, psychiatric patients at St. Elizabeth’s Hospital had dogs available for their recognized therapeutic value. And in the decades since, the medical community has come to embrace this interactive approach to improving the quality of life, both for patients in recovery and for those whose health may be in decline. For the record, today the more politically correct term for pet-related therapy is either Animal-Assisted Activities (AAA) or Animal-Assisted Therapy (AAT). AAA is a more casual meet-and-greet approach to hands-on contact between patients and pets, while AAT is a more formal clinical approach with patients who may be challenged physically, emotionally, or mentally.
PAWS FOR HEALTH Among the myriad patient services offered by Trinitas Regional Medical Center is its own Animal-Assisted Activities program, headed by Carol Pepe, Director of Case Management Services. Whether politically correct or not, everyone at Trinitas still calls it the “pet therapy program” and, indeed, this is Pepe’s pet program. She launched it almost five years ago with the approval of a multi-discipline committee of hospital representatives. To date, the AAA program’s success can be measured by the more than 3,700 visits arranged for older inpatients and cancer treatment outpatients. The Trinitas program utilizes dogs only, although many AAAs and AATs involve a variety of animals ranging from cats, birds and horses to more exotic creatures. One, in Thailand, uses elephants. The dog handlers at Trinitas are typically employee volunteers. A volunteer escort is always present, as well, to monitor overall pet–patient interaction. Currently, there are six participating therapy dogs at Trinitas: four males (Winston, Murphy, Buddy and Harley) and two females (Ribbon and Bonnie). Males and females of all breeds, including mixed, are potential candidates. Temperament always trumps sex or bloodlines. Trinitas has a close working relationship with St. Hubert’s Animal Welfare Center in Madison. Through their Paws for People program, St. Hubert’s trains and certifies both dogs and their owners/handlers. All pets are temperament-tested to assure that only appropriately friendly, stable and disciplined dogs make the cut. The owner/handler must attend a three-hour class, and both dog and owner must complete rigorous homework exercises to be certified.
THEY CALL IT PUPPY LOVE Linda Reynolds, Director of the Adult Outpatient Unit in the Department of Behavioral Health and Psychiatry, is in charge of a similar pet therapy program, which she launched only two months ago. Currently, she is the sole owner/handler of a canine “therapist,”  her five-year old beagle, Murphy. Both have been certified by St. Hubert’s. Reynolds recognized early on that Murphy had the necessary qualifications, since he had become an ambassador of goodwill in her own neighborhood, particularly among senior residents. Currently, the psych department’s group sessions are held at Trinitas, with special visits paid to the on-site nursing facility—the domain of Harley, another gifted pet “therapist.” The adult outpatient groups are often organized according to particular challenge. Two of the currently active groups are focusing on anxiety relief and partial vs. unconditional love. Reynolds refers to these sessions as her “puppy love” groups. “I really just knew I had to share him,” Reynolds says of Murphy, who wears a hospital staff photo ID badge, as do all the therapy dogs. It is attached to his favorite bandana; Reynolds realized that Murphy needed a work wardrobe and provided it. Murphy is typically on the job two or three days a month. A typical day includes sessions with two to three groups, each with five to ten patients. Patients are not the only recipients of Murphy’s healing powers. Staff members having a bad day often drop by for a visit and a pet. Murphy is happy to oblige. “No stranger is too strange for Murphy,” Reynolds says.
her five-year old beagle, Murphy. Both have been certified by St. Hubert’s. Reynolds recognized early on that Murphy had the necessary qualifications, since he had become an ambassador of goodwill in her own neighborhood, particularly among senior residents. Currently, the psych department’s group sessions are held at Trinitas, with special visits paid to the on-site nursing facility—the domain of Harley, another gifted pet “therapist.” The adult outpatient groups are often organized according to particular challenge. Two of the currently active groups are focusing on anxiety relief and partial vs. unconditional love. Reynolds refers to these sessions as her “puppy love” groups. “I really just knew I had to share him,” Reynolds says of Murphy, who wears a hospital staff photo ID badge, as do all the therapy dogs. It is attached to his favorite bandana; Reynolds realized that Murphy needed a work wardrobe and provided it. Murphy is typically on the job two or three days a month. A typical day includes sessions with two to three groups, each with five to ten patients. Patients are not the only recipients of Murphy’s healing powers. Staff members having a bad day often drop by for a visit and a pet. Murphy is happy to oblige. “No stranger is too strange for Murphy,” Reynolds says.
JUST SCRATCHING THE SURFACE The immense potential of animal-assisted therapy is particularly clear to Reynolds and Pepe, each of whom has special memories of pet–patient bonding. Pepe recalls one terminally ill patient who related incredibly to Bonnie, spending her last three weeks with regular visits. In Bonnie’s company, the patient was more relaxed and less stressed because there was no need to put on the brave face she did for family members. She even occasionally let Bonnie borrow her wig, which elicited peals of laughter from patient, handler and escort—not to mention Bonnie’s joy at being the center of so much attention. The patient was able to share some smiles and also some tears with Bonnie until the very end. Reynolds remembers a bipolar patient in a group session who had vehemently verbalized her dislike of dogs—which only encouraged Murphy to make friends. He ultimately won her heart and brought a smile to someone who hadn’t smiled in months. Pepe herself underwent surgery two years ago and became an active participant in her own program. The owner of three dogs, she experienced a case of severe pet withdrawal while in-hospital. Through some therapy dog visits, Pepe can now personally attest to the healing comfort that comes from simply petting a friendly, furry, four-legged creature. “We’re in the business of small miracles,” Pepe says. “The dogs bring smiles where before there was only pain.” EDGE
Editor’s Note: Every word you read in EDGE has to go through Christine Gibbs first. This is the first story she has authored for EDGE since joining the staff in 2009. Chris freelanced in the finance, international business and healthcare sectors as a technical writer and editor before coming aboard.
Keeping a marriage on track takes hard work and an open mind. The obstacles are unrelenting. The rewards sometimes seem few and far between. Money, job stress, child rearing and personal growth (or lack thereof) are among the big-picture challenges. Just as vexing are all the little conflicts that must be resolved merely to stay focused on moving the relationship forward. Then one day you wake up, look at your mate and wonder, “Do I really know this person?” Or worse, “Do I really know myself?” The good news is that successful couples find a way to muddle through and come out stronger on the other side. As a rule, they learn to divide their stress load as time and circumstances dictate. However, they make sure to deal with the “big stuff” as a team. This strategy is vitally important when facing the health issues that crop up as couples age. Almost every family will have to deal with a major illness at some point. How couples get through it can depend as much on their teamwork as it does on their doctors. That is why the medical field is placing increasing emphasis on providing the highest quality information and support to patient and spouse long before the physical healing process even begins.

“Patients’ emotional stability is as important as their physical well being, which is why—if and when possible—they should embark on this journey with their significant other,” says Alan P. Krieger, MD, whose patients include men undergoing prostate cancer treatment. “Couples should absolutely go through the initial steps together. Both need to understand what’s going to happen, and that works best when the doctor is able to meet both patient and partner.” Indeed, where once spouses were spared the unpleasant details of a surgical procedure—and as a result were unprepared to deal with the aftermath—now full disclosure is a crucial part of recovery.
That begins with understanding the options. For instance, most people understand that hysterectomies are performed for several reasons (ranging from unusual conditions such as ovarian carcinoma to something relatively common, such as irregular bleeding or pelvic pain). Yet they have no idea how many ways this procedure can be performed. At Trinitas Regional Medical Center, many operations—including prostate surgery and hysterectomies—are now done with the da Vinci robotic surgical system. “Good vision and maneuverability translates into more precision and a faster recovery for the patient,” says Kamran Khazaei, MD, FACOG. “The da Vinci lets surgeons see in high-definition. And by using the robotic arms with both hands, we are able to perform very delicate procedures. In many cases where patients used to need four or five days to recover, they are walking and eating the next day. In the more aggressive surgeries, recovery has been reduced from weeks to days.”
Not all cases can be addressed robotically, Khazaei cautions, ovarian cancer being one example. Likewise, not all options involve surgery. “You have to cater to each patient individually,” he says. “With medications. Injections. Therapy. As physicians, our job is to treat our patients in the least invasive way possible.” “In issues related to menopause,” he adds, “we are sensitive to the fact that women experience it, but also that men deal with it. We look for ways to keep both parties sane.” Sanity also comes into play with another medical issue that has become increasingly common among couples: Obesity. The patients treated by Joao A. Lopes, MD, and Muhammad S. Feteiha, MD, FACS, often are at the end of their rope. After years of yo-yo dieting and deteriorating health, they want to discuss a surgical option, either a gastric bypass or a gastric band. Lopes can quote the statistics on both procedures chapter and verse. Bypass patients achieve around 80 percent of the weight they anticipated losing, while band patients drop about 40 percent. That easily outweighs the option of doing nothing.

Those who fail to address their obesity in a substantial way (through diet, exercise, surgery or a combination of the three) are 300 times more likely to die 15 years earlier than people who keep their weight under control. The number that impresses Lopes most, however, is that more than 70 percent of the patients he sees come in as couples. “Success depends greatly on the understanding and support of partners and spouses,” he says. “It helps tremendously to have someone encouraging your new lifestyle, exercising with you and taking part in the process. A husband or wife must take part in their new eating behavior and move toward healthier types of foods.” As with most medical procedures, sorting through the options as a couple is the first step in a successful outcome. In the case of a band or bypass, knowing what has to happen afterwards is just as crucial. “Bariatric surgery patients really have to understand the new diet and what they’re getting into in terms of the process after surgery,” says Lopes. “The support of a spouse is tremendous, and we have a bariatric coordinator here in the office to help. Basically, we get through it together.” To help support his recovering patients, Dr. Krieger actually started the first New Jersey chapter of Us TOO, which counsels prostate cancer survivors and their partners. “My main goal is to cure the cancer,” he says, “but a key part of the recovery is for couples to know how they can work together to improve their lives and their relationship.”
Editor’s Note: Rachel Rutledge is EDGE’s ace Editorial Assistant. Lisa Milbrand, who usually writes our Healthy Edge feature, conducted the interviews for this story.
Globetrotting microbes are keeping New Jersey doctors on their toes.
There are some souvenirs you want to bring back from your travels—local handicrafts, beautiful jewelry—and then there are the ones that you don’t. These range from the inconvenient
(Montezuma’s Revenge) to the catastrophic (raging infections). Thanks to ever-adventurous New Jerseyans and newcomers from developing countries, doctors in the Garden State often find themselves treating patients with unusual, challenging-to-diagnose, and even hard-to-cure diseases. By the time they arrive at Trinitas Regional Medical Center, their condition is typically dire. Sometimes, it’s desperate.
The rundown of rare diseases that doctors are currently fighting in New Jersey includes the tropical maladies with which world travelers are now familiar. Interestingly, these are showing up less frequently. Indeed, one would expect that the incidence of, say, typhoid, malaria, and dengue fever might be on the rise. But Dr. Clark Sherer, Chief of Infectious Diseases at Trinitas, says the number of cases of these tropical diseases has remained low for the 20 years he has worked in infectious diseases.
CONFRONTING THE “CLASSICS”
“We’re not seeing more than we’re used to—just a case or two of malaria a year, and a case of dengue fever every few years,” he says.
Dr. Sherer credits the availability of immunizations and preventative medicine with keeping the numbers small. “There are people who go out into the jungle for a week on tour and never get pills to prevent malaria,” he says. “But, if you take the proper precautions regarding vaccinations, food and water, and insect and mosquito control, you can stay healthy.”
When treating some of the rarer cases, like dengue fever and typhoid, the biggest challenge for doctors can be staying abreast of the latest treatments. “Since we see them infrequently, when we make the diagnosis, we have to
familiarize ourselves with any developments in treatment,” Dr. Sherer says. “You don’t feel quite as comfortable dealing with something you only see rarely.”
TB OR NOT TB
Tuberculosis is another disease that people associate with exotic locales. And recently, headlines about drug-resistant strains of TB may have struck fear in people’s hearts. Yet Dr. Sherer says that the incidence of drug-resistant TB is relatively low.
“Tuberculosis has been out there and is still out there, but most of the cases we’re seeing are completely sensitive to treatment,” he maintains.
While the number of cases of TB has grown, Dr. Sherer says there’s little need for the general public to worry. “Most of the cases we’re seeing here are in foreign-born people who are on the younger side. They were exposed in another country where TB is endemic, and later develop active TB.”
BAD BUGS
The most challenging cases the doctors are seeing involve bacterial infections, whether it’s unusual strains of mycobacteria brought back from a trip to a developing country or the homegrown variety of infections that are antibiotic-resistant.
Necrotizing fasciitis—a rapidly spreading infection that can kill off large swaths of soft tissue in a matter of hours— can be especially life-threatening.
“They have to be treated surgically immediately,” says Dr. Morteza Khaladj of The Center for Wound Healing and Hyperbaric Medicine. “We clean and drain the infection. Sometimes we have to remove the bone and large sections of soft tissue. Then patients are treated with IV antibiotics.”
The most troubling new infectious disease—methicillin-resistant Staphylococcus aureus (MRSA)— started right in our own backyard. MRSA began cropping up in hospitals as people with weakened immune systems began to develop
antibiotic-resistant staph infections in the skin, which often spread to surgical wounds, bones, and joints, and even into the major organs. This new strain of Staph infection has grown resistant to many antibiotics. Then a new strain developed—community-acquired MRSA—which can cause skin infections and pneumonia.
“Healthy people are coming into the hospital with overwhelming staph infections, very resistant strains of E. coli and other bacteria—some are resistant to all antibiotics,” Dr. Sherer says. “It’s a big concern—there are not many new antibiotics out there, so our resources are limited in treating some of these infections. MRSA has become a huge issue that we’re dealing with on a daily basis.”

So should you be worried? Most medical experts say that with the proper precautions, you can get through life safely, whether you’re jetting halfway around the world or driving to the local Wawa for a quart of milk.
“I don’t think the average person needs to be concerned,” Dr. Sherer says. “Just follow the CDC’s recommendations regarding the precautions you should take when you travel someplace where you might be at risk, and you should be fine.”