I’m so tired, I haven’t slept a wink… I’m so tired, my mind is on the blink.

Photo credit: iStockphoto/Thinkstock
Beatles aficionados will recognize these lyrics from the Let It Be album. Truth be told, the group’s weary words should resonate with anyone who has ever been sleep-deprived for more than a night or two. The fact is, we’ve all been there—from punching the snooze button for an extra five minutes, to skipping that 5:45 a.m. spin class in hope of additional Zs, to heading straight for the couch after a long workday. So why is feeling fatigued so common? Why is having a healthy sleep so important? And what would be the downside if we just let it be? Health and sleep are inherently intertwined. Sleeping is a regenerative process for both the mind and body. A sufficient amount of quality slumber helps to maintain a healthy heart, metabolism and endocrine system.
Since most of us spend one-third of our lives buried in a pillow, it is important to have healthy and consistent sleep on a regular nightly basis. For some, however, nights featuring the cardinal eight hours are few and far between. According to the National Heart, Lung and Blood Institute, about 70 m llion people in the U.S. have a sleep problem and 40 million of these are chronic problems. Maybe you are a habitual snorer; you wake in the night and have difficulty falling back asleep; you’ve gained a significant amount of weight in the past year; or you kick during sleep. All of these symptoms and more can be associated with sleep disorders, though they are often under-diagnosed. All are curable. If left untreated, however, they can lead to serious health issues. Insomnia (the inability to fall asleep or stay asleep), for example, results in loss of concentration, reduced productivity and poor alertness.
Over time, insufficient sleep creates chaos within metabolic hormones, which can lead to obesity and diabetes. Sleep Apnea (breathing stoppage and diminished oxygen levels) can affect one’s blood pressure, heart and brain. It can lead to serious cardiovascular complications, including hypertension and strokes. While sleep disorders are prevalent in adults, they are increasing for children. If untreated, children may experience emotional, behavioral and learning disorders. As with most diseases, the symptoms triggered by sleep disorders can escalate over time. That being said, not all sleep-related difficulties are actually classified as disorders. There are many modifications that can be performed to improve sleep habits, such as shortening naps, avoiding caffeine and alcohol, and fixing a bedtime and wake-up time.
SEEING A SPECIALST If making a few lifestyle changes doesn’t do the trick, the next move is seeing a sleep specialist and undergoing a sleep study, which can diagnose and ultimately cure the disorder. Unfortunately, many people shy away from submitting to this type of procedure. They picture themselves in a bleak hospital sub-basement, on an uncomfortable cot, with wires connecting them to a bank of machines. The reality is quite different. At the Trinitas Comprehensive Sleep Disorders Center, for example, homey bedrooms await the troubled sleeper. The state-of- the-art facility offers monitored diagnostic sleep studies that are designed to quickly reveal the disorder. Trained sleep specialists and technicians work together on each study and conduct follow-up appointments with a subject’s physician. All cases are reviewed by Dr. Vipin Garg, the center’s Medical Director. Dr. Garg is board- certified as a Sleep Specialist, as well as in Pulmonary Medicine, Critical Care and Internal Medicine.
One of the center’s goals is to make patients feel as comfortable as possible during their stay. The center on the TRMC campus consists of four bedrooms—each with a personal bathroom and television and other amenities. To fulfill the growth and demand for more space, the center expanded to the Homewood Suites by Hilton in Cranford early in 2010. There are now two fully equipped bedrooms at this property. Dr. Garg notes how important it is to feel comfortable and at ease during a sleep study in order to gather the most helpful results. “The psychological mind-state of sleeping in a center is not the same as being at home,” he explains. “We try to make it feel as if you are in a hotel, rather than a hospital. We have access to all resources from the hospital’s many departments, and facilities at the hotel are extended to patients, including breakfast and the gym.” Sleep studies and treatment provided at the center are personalized for each type of sleep disorder. The staff is certified and trained in many disciplines and an array of treatment options is available.
If the problem is neurological, a neurologist will meet with the patient. For breathing issues, a pulmonologist will be present. If significant weight-loss is deemed beneficial to a sleep apnea patient, dieticians and surgery options are at hand. All sleep disorders are curable and patients have the opportunity to choose from treatment types. For example, if diagnosed with sleep apnea, depending on the case, one can undergo surgery for tonsil removal or sleep with a CPAP machine, which delivers additional air through the nose.
ONE NIGHT ONLY Typically, a single night of monitoring can result in a lifetime of quality sleep. The process is simple. Patients are instructed to do what they would typically do before any night of sleep, to ensure regularity and comfort, such as reading or watching TV. Patients are hooked up to leads that measure eye and leg movement, heart rate, airflow measurements and more—all while specialists watch the sleep behavior on video monitors. After roughly one week, the patients are asked to come back, results are reported and treatment  arrangements are made. For those who cannot (or will not) leave home to participate in a study, Dr. Garg proposes an alternative possibility: an at-home sleep study, using a new portable device that collects the same useful data. Success stories are hardly few and far between at Trinitas Comprehensive Sleep Disorders Center. On the contrary, the center conducted nearly 1,500 studies in 2012, including adults and children. One of Dr. Garg’s favorite stories concerns an eight-year-old boy, who was prescribed ADHD medication after meeting with a psychiatrist and pediatrician for hyperactivity and inattention in school.
arrangements are made. For those who cannot (or will not) leave home to participate in a study, Dr. Garg proposes an alternative possibility: an at-home sleep study, using a new portable device that collects the same useful data. Success stories are hardly few and far between at Trinitas Comprehensive Sleep Disorders Center. On the contrary, the center conducted nearly 1,500 studies in 2012, including adults and children. One of Dr. Garg’s favorite stories concerns an eight-year-old boy, who was prescribed ADHD medication after meeting with a psychiatrist and pediatrician for hyperactivity and inattention in school.
The boy’s mother mentioned his nightly snoring to the pediatrician, who recommended a sleep study. Dr. Garg diagnosed a severe case of Obstructive Sleep Apnea. After addressing the apnea, the ADHD medications were no longer needed, the boy’s performance in school drastically improved, and he became more energetic after losing weight. “The importance of sleep is an issue that has been previously ignored,” Dr. Garg laments. “Many times an internist fails to realize sleep disorders may be the problem at hand, because different questions are asked during a physical than during a sleep study. The impact of a sleep study is huge. It is a very natural, non-invasive process with no known side effects. The technology is getting better day by day, and we have had a lot of success.” Healthy sleep is imperative for us as individuals. By diagnosing and treating a sleep disorder, future serious issues can be avoided. The Trinitas Comprehensive Sleep Disorders Center is one of many centers that can help in the journey of pursuing quality sleep habits. Don’t let it be. If you are experiencing sleep difficulties, talk to your physician or sleep specialist about a center near you, and get on the road to a dreamy recovery.
Editor’s Note: The Trinitas Comprehensive Sleep Disorder Center is accredited by the American Academy of Sleep Medicine. It is located at 210 Williamson St. in Elizabeth. For more information, call 908.994.8694 or log onto njsleepdisorderscenter.com.


 sure you are on-track to reach your goals.
sure you are on-track to reach your goals.
 Editor’s Note: Gerontologist Alexis Abramson, PhD appears frequently as an on-air expert for NBC’s Today show, and also on CNN, CBS and MSNBC. Her commitment to baby boomers and mature adults has been featured in TIME, Forbes, The Wall Street Journal, People and other national publications. To see more of her thoughts on aging gracefully (and intelligently), log onto alexisabramson.com.
Editor’s Note: Gerontologist Alexis Abramson, PhD appears frequently as an on-air expert for NBC’s Today show, and also on CNN, CBS and MSNBC. Her commitment to baby boomers and mature adults has been featured in TIME, Forbes, The Wall Street Journal, People and other national publications. To see more of her thoughts on aging gracefully (and intelligently), log onto alexisabramson.com.
 Flip-Flopping in the Classroom The back-to-school season always holds some surprises for educators, kids and parents. This year, many noticed a rise in foot pain among returning students. The popularity of cheap, stylish flip-flops has more than a little to do with this, according to the American College of Foot and Ankle Surgeons. Right into the mid-teens, kids have new bone growing in their heels. Flip-flops offer no support or cushioning for this part of the foot, and summer-long repetitive stress can manifest itself in pain and injuries once students switch back to traditional school footwear. If your child is experiencing pain, it’s important to explore an immediate remedy—stretching exercises, ice massage, anti-inflammatory medications, and custom or over-the-counter shoe inserts are certainly worth exploring. Obviously, if the pain worsens or persists, a visit to the podiatrist is called for.
Flip-Flopping in the Classroom The back-to-school season always holds some surprises for educators, kids and parents. This year, many noticed a rise in foot pain among returning students. The popularity of cheap, stylish flip-flops has more than a little to do with this, according to the American College of Foot and Ankle Surgeons. Right into the mid-teens, kids have new bone growing in their heels. Flip-flops offer no support or cushioning for this part of the foot, and summer-long repetitive stress can manifest itself in pain and injuries once students switch back to traditional school footwear. If your child is experiencing pain, it’s important to explore an immediate remedy—stretching exercises, ice massage, anti-inflammatory medications, and custom or over-the-counter shoe inserts are certainly worth exploring. Obviously, if the pain worsens or persists, a visit to the podiatrist is called for. Follow-Up on NYC Soda Ban New York’s short-lived soda ban spurred a slew of studies on the actual impact of obesity-focused legislation. A recent article published in the American Journal of Agricultural Economics suggests that strategies such as taxing sugary beverages would not reduce obesity, because consumers would simply switch to un-taxed options. Public health advocates have posited that higher prices would deter unhealthy food purchases. But according to research economists, that simply isn’t the case. In New York, a court ruled that the Board of Health exceeded its authority in instituting the ban, which was pushed by Mayor Michael Bloomberg. Among the criticisms of an “obesity tax” is that it would target lower-income consumers who tend to buy more high-calorie foods and beverages, and thus would be a regressive tax. Even so, the search for a “social solution” will continue; more than a third of U.S. adults, and one in six children, are technically obese. The medical costs associated with obesity are between $125 and $150 billion a year.
Follow-Up on NYC Soda Ban New York’s short-lived soda ban spurred a slew of studies on the actual impact of obesity-focused legislation. A recent article published in the American Journal of Agricultural Economics suggests that strategies such as taxing sugary beverages would not reduce obesity, because consumers would simply switch to un-taxed options. Public health advocates have posited that higher prices would deter unhealthy food purchases. But according to research economists, that simply isn’t the case. In New York, a court ruled that the Board of Health exceeded its authority in instituting the ban, which was pushed by Mayor Michael Bloomberg. Among the criticisms of an “obesity tax” is that it would target lower-income consumers who tend to buy more high-calorie foods and beverages, and thus would be a regressive tax. Even so, the search for a “social solution” will continue; more than a third of U.S. adults, and one in six children, are technically obese. The medical costs associated with obesity are between $125 and $150 billion a year. Drug Wonder Downunder A pair of Australian medical researchers have been recognized for their breakthrough work with Duchenne Muscular Dystrophy, a condition caused by mutations in the dystrophin gene on the X chromosome—which means it mostly affects boys. DMD patients are wheelchair-dependent by age 12 and often don’t survive past their early 20s. The researchers have developed a drug that works by skipping over the faulty part of the gene, producing a functional version of the protein dystrophin. This protein stabilizes the muscle fiber during muscle contraction. Without dystrophin, muscle fibers are replaced by scar tissue. In clinical trials, boys on the drugs have been walking up hills, operating pedal cars and whistling after 90 weeks. “It is extremely exciting to see that genetic testing is finally coming to the forefront of clinical medicine,” says Dr. Kevin Lukenda, Chairman of TRMC’s Family Medicine Department. “For years, this information was limited to research and academia. With a simple swab of a patient’s saliva in my office, we can detect over 30 possible genetic mutations within an individual’s DNA. This is the future of early diagnoses and treatment in clinical medicine.”
Drug Wonder Downunder A pair of Australian medical researchers have been recognized for their breakthrough work with Duchenne Muscular Dystrophy, a condition caused by mutations in the dystrophin gene on the X chromosome—which means it mostly affects boys. DMD patients are wheelchair-dependent by age 12 and often don’t survive past their early 20s. The researchers have developed a drug that works by skipping over the faulty part of the gene, producing a functional version of the protein dystrophin. This protein stabilizes the muscle fiber during muscle contraction. Without dystrophin, muscle fibers are replaced by scar tissue. In clinical trials, boys on the drugs have been walking up hills, operating pedal cars and whistling after 90 weeks. “It is extremely exciting to see that genetic testing is finally coming to the forefront of clinical medicine,” says Dr. Kevin Lukenda, Chairman of TRMC’s Family Medicine Department. “For years, this information was limited to research and academia. With a simple swab of a patient’s saliva in my office, we can detect over 30 possible genetic mutations within an individual’s DNA. This is the future of early diagnoses and treatment in clinical medicine.” You Snooze, You Lose Don’t lose sleep over junk food purchases. Seriously, don’t. A new study shows that lack of sleep can lead people to buy more food—and more high-calorie items— when they shop. Researchers gave 14 normal-weight men a budget of $50 and instructed them to purchase as much as they could out of a possible 40 food items, which included 20 high-calorie and 20 low-calorie foods. They conducted this exercise after a night of sleep deprivation and again after a good night’s sleep. They bought 18 percent more food— and 9 percent more calories—after a night of sleep deprivation. “Another recent study showed tha
You Snooze, You Lose Don’t lose sleep over junk food purchases. Seriously, don’t. A new study shows that lack of sleep can lead people to buy more food—and more high-calorie items— when they shop. Researchers gave 14 normal-weight men a budget of $50 and instructed them to purchase as much as they could out of a possible 40 food items, which included 20 high-calorie and 20 low-calorie foods. They conducted this exercise after a night of sleep deprivation and again after a good night’s sleep. They bought 18 percent more food— and 9 percent more calories—after a night of sleep deprivation. “Another recent study showed tha t the pleasure centers of the brain were activated more when sleep-deprived people looked at pictures of junk food,” adds Dr. Vipin Garg, Director of the Trinitas Comprehensive Sleep Disorders Center. “Lack of sleep can prevent the brain from making an intelligent decision regarding healthy food choices. Getting enough quality sleep can help weight control by allowing people to make proper nutritional decisions and also provide energy to exercise to achieve better overall health.” There are plans in the works for follow-up studies to see how sleep deprivation affects other buying decisions.
t the pleasure centers of the brain were activated more when sleep-deprived people looked at pictures of junk food,” adds Dr. Vipin Garg, Director of the Trinitas Comprehensive Sleep Disorders Center. “Lack of sleep can prevent the brain from making an intelligent decision regarding healthy food choices. Getting enough quality sleep can help weight control by allowing people to make proper nutritional decisions and also provide energy to exercise to achieve better overall health.” There are plans in the works for follow-up studies to see how sleep deprivation affects other buying decisions. Word of Mouth Unreliable Where Strokes are Concerned So what’s the deal with the “Crooked Tongue” story making the rounds on social media? According to countless emails and Facebook postings, a woman who was suffering from a stroke but didn’t exhibit the typical symptoms was diagnosed by an alert ER physician who asked her to stick out her tongue. When she did so, and her tongue presented to one side rather than straight out, he was able to correctly diagnose the stroke and save his patient’s life. Is the “crooked tongue” technique a reliable way to diagnose stroke? According to Dr. John D’Angelo, Chairman of Trinitas Regional Medical Center’s Emergency Department, the story has all the earmarks of an urban legend. “I can find no reference to this suggestion from any reliable source, such as the Heart and Stroke Foundation, the American Heart Association or the National Institute of Neurological Disorders and Stroke,” he says. “Lingual deviation can indicate a host of issues that are typically associated with a tumor or other type of lesion. So a crooked tongue is a sign that something is wrong, but it’s not a reliable sign you are having a stroke.” The T in the American Stroke Assoc
Word of Mouth Unreliable Where Strokes are Concerned So what’s the deal with the “Crooked Tongue” story making the rounds on social media? According to countless emails and Facebook postings, a woman who was suffering from a stroke but didn’t exhibit the typical symptoms was diagnosed by an alert ER physician who asked her to stick out her tongue. When she did so, and her tongue presented to one side rather than straight out, he was able to correctly diagnose the stroke and save his patient’s life. Is the “crooked tongue” technique a reliable way to diagnose stroke? According to Dr. John D’Angelo, Chairman of Trinitas Regional Medical Center’s Emergency Department, the story has all the earmarks of an urban legend. “I can find no reference to this suggestion from any reliable source, such as the Heart and Stroke Foundation, the American Heart Association or the National Institute of Neurological Disorders and Stroke,” he says. “Lingual deviation can indicate a host of issues that are typically associated with a tumor or other type of lesion. So a crooked tongue is a sign that something is wrong, but it’s not a reliable sign you are having a stroke.” The T in the American Stroke Assoc
 promise for a more effective treatment of Type 2 Diabetes, which currently affects more than 25 million Americans. In the Harvard study, Belatrophin caused mice to produce insulin-secreting pancreatic beta cells at up to 30 times the normal rate. The new cells produce insulin only when called upon by the body. This offers the potential for natural regulation of insulin, as well as a reduction in the complications associated with diabetes. There is hope that this treatment may also have an impact on juvenile diabetes. It could eventually mean that instead of taking insulin injections three times a day, you might take an injection of this hormone once a week or once a month or—in the best case—maybe even once a year, explains Doug Melton, one of the researchers. “This new hormone offers optimism for researchers lo
promise for a more effective treatment of Type 2 Diabetes, which currently affects more than 25 million Americans. In the Harvard study, Belatrophin caused mice to produce insulin-secreting pancreatic beta cells at up to 30 times the normal rate. The new cells produce insulin only when called upon by the body. This offers the potential for natural regulation of insulin, as well as a reduction in the complications associated with diabetes. There is hope that this treatment may also have an impact on juvenile diabetes. It could eventually mean that instead of taking insulin injections three times a day, you might take an injection of this hormone once a week or once a month or—in the best case—maybe even once a year, explains Doug Melton, one of the researchers. “This new hormone offers optimism for researchers lo
 University of Oregon’s Department of Psychology, learning meditation techniques makes it easier for smokers to taper off. Mindful Meditation—a technique that encourages people to relax, focus on the current moment and “go with the flow” of thoughts and sensation—has already been shown to have a positive impact on cold and flu, hot flashes and irritable bowel syndrome. In the Oregon study, 60 people received five hours of either relaxation training or Mindful Meditation training. Among the smokers in the study, there was no difference in the amount the relaxation group smoked. However, the smokers in the meditation group had cut back by 60 percent. Researchers admit that the smoking findings are surprising, and caution that the study was very small. Also, the participants were all college students. On the other hand, none of the subjects were told they were taking part in a smoking study. And the Oregon study found that the brains of the smokers who learned meditation techniques were more active in an area linked to self-control. More work in this area is warranted.
University of Oregon’s Department of Psychology, learning meditation techniques makes it easier for smokers to taper off. Mindful Meditation—a technique that encourages people to relax, focus on the current moment and “go with the flow” of thoughts and sensation—has already been shown to have a positive impact on cold and flu, hot flashes and irritable bowel syndrome. In the Oregon study, 60 people received five hours of either relaxation training or Mindful Meditation training. Among the smokers in the study, there was no difference in the amount the relaxation group smoked. However, the smokers in the meditation group had cut back by 60 percent. Researchers admit that the smoking findings are surprising, and caution that the study was very small. Also, the participants were all college students. On the other hand, none of the subjects were told they were taking part in a smoking study. And the Oregon study found that the brains of the smokers who learned meditation techniques were more active in an area linked to self-control. More work in this area is warranted.
 Painkiller Overdoses Spiking Among Women A new report from the Centers for Disease Control offers some eye-opening facts on the abuse of painkillers among women. Since 1999, the number of women who have died from a painkiller overdose has increased by a factor of four. “Mothers, wives, sisters, and daughters are dying at rates that we have never seen before,” says Dr. Thomas Frieden, Director of the CDC. Among the more alarming aspects of the report are: 1) On average, 18 women die
Painkiller Overdoses Spiking Among Women A new report from the Centers for Disease Control offers some eye-opening facts on the abuse of painkillers among women. Since 1999, the number of women who have died from a painkiller overdose has increased by a factor of four. “Mothers, wives, sisters, and daughters are dying at rates that we have never seen before,” says Dr. Thomas Frieden, Director of the CDC. Among the more alarming aspects of the report are: 1) On average, 18 women die  from painkiller overdoses in the U.S. every day; 2) More women die from prescription drug overdoses than from car accidents; 3) Some 50,000 women between the ages of 25 and 34 will be taken to U.S. emergency rooms as a result of painkiller overdoses this year. In its report, the CDC recommended that healthcare providers exercise greater caution when prescribing prescription medications—and suggested that states and the federal government could turn this trend around by doing a better job educating women on the dangers of prescription painkillers. “We are seeing an increase in the numbers of women and young people presenting in the emergency room with prescription pain and anxiety medications—many of whom have legitimate prescriptions for a physical or mental health disorder, and others who are accessing prescription meds from others or on the street,” Lisa Dressner confirms. Dressner is Program Director of TRMC’s Psychiatric Emergency Services. “Too often, alternatives to these highly addictive medications are not explored, and primary care or pain management doctors may not fully assess someone’s potential or history of substance abuse.” There is an urgent need, she adds, for more education to consumers around the potential for addiction to commonly prescribed pain meds, and medications for problems related to anxiety or sleep, so that risk for abuse of these medications, and increased depression, withdrawal and suicidality is minimized.
from painkiller overdoses in the U.S. every day; 2) More women die from prescription drug overdoses than from car accidents; 3) Some 50,000 women between the ages of 25 and 34 will be taken to U.S. emergency rooms as a result of painkiller overdoses this year. In its report, the CDC recommended that healthcare providers exercise greater caution when prescribing prescription medications—and suggested that states and the federal government could turn this trend around by doing a better job educating women on the dangers of prescription painkillers. “We are seeing an increase in the numbers of women and young people presenting in the emergency room with prescription pain and anxiety medications—many of whom have legitimate prescriptions for a physical or mental health disorder, and others who are accessing prescription meds from others or on the street,” Lisa Dressner confirms. Dressner is Program Director of TRMC’s Psychiatric Emergency Services. “Too often, alternatives to these highly addictive medications are not explored, and primary care or pain management doctors may not fully assess someone’s potential or history of substance abuse.” There is an urgent need, she adds, for more education to consumers around the potential for addiction to commonly prescribed pain meds, and medications for problems related to anxiety or sleep, so that risk for abuse of these medications, and increased depression, withdrawal and suicidality is minimized. other developed countries. Only a third of American girls have been fully vaccinated; in other countries (including Rwanda!) the rate is closer to 80 percent. HPV causes 19,000 cases of cancer among women in the U.S. each year. It also accounts for 8,000 cases in men, a statistic brought to light by actor Michael Douglas, whose throat cancer was identified as being HPV-related. “The study showed that less than four years later the prevalence of the vaccine strains among young women aged 14–19 years had fallen by 56%,” points out Dr. William Farrer, Associate Program Director and Associate Professor of Medicine of the Seton Hall University School of Health and Medical Sciences at TRMC. “This was despite the fact that in 2010, only 32% of 13–17 year-olds had received the full 3-dose series of vaccine. Rates of HPV infection in older women had not fallen, probably reflecting the fact that they were not the target group for the vaccine.The researchers also reported that ‘Sexual behavior among females aged 14–19 years overall was similar in the two periods.’ This should reassure opponents of the HPV vaccine who expressed concern that somehow use of the vaccine would encourage promiscuity.”
other developed countries. Only a third of American girls have been fully vaccinated; in other countries (including Rwanda!) the rate is closer to 80 percent. HPV causes 19,000 cases of cancer among women in the U.S. each year. It also accounts for 8,000 cases in men, a statistic brought to light by actor Michael Douglas, whose throat cancer was identified as being HPV-related. “The study showed that less than four years later the prevalence of the vaccine strains among young women aged 14–19 years had fallen by 56%,” points out Dr. William Farrer, Associate Program Director and Associate Professor of Medicine of the Seton Hall University School of Health and Medical Sciences at TRMC. “This was despite the fact that in 2010, only 32% of 13–17 year-olds had received the full 3-dose series of vaccine. Rates of HPV infection in older women had not fallen, probably reflecting the fact that they were not the target group for the vaccine.The researchers also reported that ‘Sexual behavior among females aged 14–19 years overall was similar in the two periods.’ This should reassure opponents of the HPV vaccine who expressed concern that somehow use of the vaccine would encourage promiscuity.” Air Pollution Linked to Sleep Disorders in Children While we watch the Arab Spring unfold in Egypt in dramatic fashion, some dramatic health news has come out of that country that is relevant right here in New Jersey. In July, University of Cairo researchers announced the results of sleep study on school-age children, which shows a link between air pollution and sleep disorders. The 276 children in the study exhibited significant disorders of initiating and maintaining sleep, and excessive
Air Pollution Linked to Sleep Disorders in Children While we watch the Arab Spring unfold in Egypt in dramatic fashion, some dramatic health news has come out of that country that is relevant right here in New Jersey. In July, University of Cairo researchers announced the results of sleep study on school-age children, which shows a link between air pollution and sleep disorders. The 276 children in the study exhibited significant disorders of initiating and maintaining sleep, and excessive  somnolence when exposed to PM10 (particulate matter smaller than 10 micrometers) in the air. PM10 particles can settle in the lungs and cause health problems. Larger particles are typically filtered by the nose and throat. In treating the pediatric population at the Trinitas Comprehensive Sleep Disorders Center, Vipin Garg, MD, Director of the Center notes that, “Small particles or large particles of pollution can irritate the airways of children, especially those who have large adenoids. Children who have to breathe through their mouths because of enlarged adenoids bypass the normal filtering process of the nose and that can have an irritant effect on both the upper and lower airways. This may result in a significant sleep disturbance especially if sleep is already compromised. Also lower airway irritation can lead to asthma-like symptoms.”
somnolence when exposed to PM10 (particulate matter smaller than 10 micrometers) in the air. PM10 particles can settle in the lungs and cause health problems. Larger particles are typically filtered by the nose and throat. In treating the pediatric population at the Trinitas Comprehensive Sleep Disorders Center, Vipin Garg, MD, Director of the Center notes that, “Small particles or large particles of pollution can irritate the airways of children, especially those who have large adenoids. Children who have to breathe through their mouths because of enlarged adenoids bypass the normal filtering process of the nose and that can have an irritant effect on both the upper and lower airways. This may result in a significant sleep disturbance especially if sleep is already compromised. Also lower airway irritation can lead to asthma-like symptoms.” Walking the Walk While the medical profession has long promoted the benefits of daily exercise, a new study out of the Middle East pinpoints how short, brisk walks taken after meals are an effective way to diminish the risk of developing Type 2 diabetes. The results, published in the latest issue of Diabetes Care, focus on how post-meal strolls reduce blood sugar levels. “Blood sugar levels are the highest after meals and as we age our pancreas is less effective in releasing insulin, a hormone that helps lower blood sugar,”
Walking the Walk While the medical profession has long promoted the benefits of daily exercise, a new study out of the Middle East pinpoints how short, brisk walks taken after meals are an effective way to diminish the risk of developing Type 2 diabetes. The results, published in the latest issue of Diabetes Care, focus on how post-meal strolls reduce blood sugar levels. “Blood sugar levels are the highest after meals and as we age our pancreas is less effective in releasing insulin, a hormone that helps lower blood sugar,”  explains Dr. Mahmoud Ali Zirie, who ran the study out of Qatar. “This leads to higher blood sugar that can increase the risk of diabetes. A short walk two hours after meals can help normalize blood sugar levels. To achieve maximum health benefits walking should be moderate intensity. In other words, it needs to be faster than a stroll and brisk enough to raise your heart rate.” Those who are new to this type of exercise should begin slowly, stay hydrated and avoid excessive heat, and build toward a regular and rigorous regimen. Kathleen McCarthy, RN, a Certified Diabetes Educator at Trinitas, offers these tips: “Whether you have diabetes or you are trying to keep diabetes at arm’s length, you will benefit from a regular exercise regimen of 30 minutes a day, five days a week, or more. Short brisk walks, two hours after a meal, improve post-prandial (after meal) glucose readings. Walking also improves circulation, heart and lung function, and releases endorphins which help control of stress and pain. As you build muscle mass, your metabolism will increase which then gives you more energy and will lead to weight loss over time. The benefits of aerobic exercise last up to 12 hours after exercise. Exercise is a key ingredient to improve or maintain optimal health.”
explains Dr. Mahmoud Ali Zirie, who ran the study out of Qatar. “This leads to higher blood sugar that can increase the risk of diabetes. A short walk two hours after meals can help normalize blood sugar levels. To achieve maximum health benefits walking should be moderate intensity. In other words, it needs to be faster than a stroll and brisk enough to raise your heart rate.” Those who are new to this type of exercise should begin slowly, stay hydrated and avoid excessive heat, and build toward a regular and rigorous regimen. Kathleen McCarthy, RN, a Certified Diabetes Educator at Trinitas, offers these tips: “Whether you have diabetes or you are trying to keep diabetes at arm’s length, you will benefit from a regular exercise regimen of 30 minutes a day, five days a week, or more. Short brisk walks, two hours after a meal, improve post-prandial (after meal) glucose readings. Walking also improves circulation, heart and lung function, and releases endorphins which help control of stress and pain. As you build muscle mass, your metabolism will increase which then gives you more energy and will lead to weight loss over time. The benefits of aerobic exercise last up to 12 hours after exercise. Exercise is a key ingredient to improve or maintain optimal health.” Mild Depression and Alzheimer’s A recent aging study conducted by researchers in the U.S. and Asia has found that the onset of Alzheimer’s Disease appears to be accelerated by depression. The study suggested that individuals with depressive symptoms progressed from mild cognitive impairment to full-blown Alzheimer’s at a much faster rate than those who did not exhibit signs of depression. Indeed, depression doubled the risk of developing Alzheimer’s in this particular study. These findings have opened
Mild Depression and Alzheimer’s A recent aging study conducted by researchers in the U.S. and Asia has found that the onset of Alzheimer’s Disease appears to be accelerated by depression. The study suggested that individuals with depressive symptoms progressed from mild cognitive impairment to full-blown Alzheimer’s at a much faster rate than those who did not exhibit signs of depression. Indeed, depression doubled the risk of developing Alzheimer’s in this particular study. These findings have opened  up a number of debates about what actually triggers the cognitive decline. However, it strongly suggests that decisive steps to intervene or mediate depression among people at risk for Alzheimer’s need to be taken. “Occasionally, depression in the elderly, even in the absence of dementia, has been known to result in impairment of cognitive functions,” adds Dr. Anwar Y. Ghali, Chairman of Psychiatry at Trinitas. “Especially the memory, in a condition referred to as ‘depressive pseudo dementia.’ Hence, one would expect that this might occur at a higher rate with patients already diagnosed with Alzheimer’s. Therefore, physicians should always evaluate Alzheimer’s patients for the possibility of a co-morbid depression. With adequate treatment of depression, patients should be relieved of suffering and also experience reduced possibility of suicide—a complication of depression that occurs at a higher rate with the elderly, especially in males and particularly for those suffering from an additional illness.”
up a number of debates about what actually triggers the cognitive decline. However, it strongly suggests that decisive steps to intervene or mediate depression among people at risk for Alzheimer’s need to be taken. “Occasionally, depression in the elderly, even in the absence of dementia, has been known to result in impairment of cognitive functions,” adds Dr. Anwar Y. Ghali, Chairman of Psychiatry at Trinitas. “Especially the memory, in a condition referred to as ‘depressive pseudo dementia.’ Hence, one would expect that this might occur at a higher rate with patients already diagnosed with Alzheimer’s. Therefore, physicians should always evaluate Alzheimer’s patients for the possibility of a co-morbid depression. With adequate treatment of depression, patients should be relieved of suffering and also experience reduced possibility of suicide—a complication of depression that occurs at a higher rate with the elderly, especially in males and particularly for those suffering from an additional illness.” Landmark Diabetes Study Completed The recently completed Look AHEAD study by the University of Pittsburgh has brought into question the value of lifestyle intervention programs for overweight and obese Type 2 diabetes patients. The study covered more than 5,000 people at 16 clinical centers across the country, over more than a decade. One group in the study followed an aggressive program of weight management and increased physical activity. The other was only provided with health information and support related to diabetes. In terms of strokes and heart attacks, there was no significant difference between the two groups. The biggest difference between the groups was in the area of weight loss. The information and support group lost relatively little weight, while the intervention group lost 8.7 percent of their body weight and had excellent success keeping it off. A 5 percent weight loss is considered clinically significant, particularly in the controlling of cholesterol, blood pressure and blood sugar. “While the findings from the Look AHEAD study did not support that
Landmark Diabetes Study Completed The recently completed Look AHEAD study by the University of Pittsburgh has brought into question the value of lifestyle intervention programs for overweight and obese Type 2 diabetes patients. The study covered more than 5,000 people at 16 clinical centers across the country, over more than a decade. One group in the study followed an aggressive program of weight management and increased physical activity. The other was only provided with health information and support related to diabetes. In terms of strokes and heart attacks, there was no significant difference between the two groups. The biggest difference between the groups was in the area of weight loss. The information and support group lost relatively little weight, while the intervention group lost 8.7 percent of their body weight and had excellent success keeping it off. A 5 percent weight loss is considered clinically significant, particularly in the controlling of cholesterol, blood pressure and blood sugar. “While the findings from the Look AHEAD study did not support that  engagement in a weight-loss intervention was effective for reducing the onset of cardiovascular disease incidence or mortality, this does not mean that overweight adults with diabetes should not lose weight and become more physically active,” says John Jakicic of the Department of Health and Physical Activity in Pitt’s School of Education. Dr. Ari Eckman, Chief of Endocrinology and Metabolism at Trinitas, adds that there is an overwhelming amount of evidence from this study to date that has shown that weight loss and physical activity were associated with numerous other health benefits: “While weight loss alone was not shown to significantly decrease this incidence in the recent Look AHEAD study, there is strong support from numerous studies supporting the benefits of weight loss and physical activity for many other health benefits. Further studies are recommended to determine the full effect weight loss has on cardiovascular disease prevention. It is still strongly recommended for people with diabetes who are overweight or obese to lose weight and maintain a healthy lifestyle.”
engagement in a weight-loss intervention was effective for reducing the onset of cardiovascular disease incidence or mortality, this does not mean that overweight adults with diabetes should not lose weight and become more physically active,” says John Jakicic of the Department of Health and Physical Activity in Pitt’s School of Education. Dr. Ari Eckman, Chief of Endocrinology and Metabolism at Trinitas, adds that there is an overwhelming amount of evidence from this study to date that has shown that weight loss and physical activity were associated with numerous other health benefits: “While weight loss alone was not shown to significantly decrease this incidence in the recent Look AHEAD study, there is strong support from numerous studies supporting the benefits of weight loss and physical activity for many other health benefits. Further studies are recommended to determine the full effect weight loss has on cardiovascular disease prevention. It is still strongly recommended for people with diabetes who are overweight or obese to lose weight and maintain a healthy lifestyle.”

 Don’t Just Sit There! Thanks to a new study out of Australia, you can add one more thing to the list of long-term health no-no’s that includes smoking, drinking, lack of exercise and a high-fat diet: Sitting. Research by the Sax Institute of adults 45 and over found that those who sat for 11 or more hours a day had a 40% higher risk of dying within the next three years than people who sat less than four hours a day. The study adjusted for an array of other lifestyle and medical issues, but even for those who exercised regularly, the risk of death still rose with every additional hour spent in a chair.
Don’t Just Sit There! Thanks to a new study out of Australia, you can add one more thing to the list of long-term health no-no’s that includes smoking, drinking, lack of exercise and a high-fat diet: Sitting. Research by the Sax Institute of adults 45 and over found that those who sat for 11 or more hours a day had a 40% higher risk of dying within the next three years than people who sat less than four hours a day. The study adjusted for an array of other lifestyle and medical issues, but even for those who exercised regularly, the risk of death still rose with every additional hour spent in a chair. New Road Map for Families of Teen Diabetics For many parents, coping day-to-day with their teenagers is the most difficult, aggravating and exhausting phase of the child-rearing process. For parents of teens with Type 1 Diabetes, managing the disease and the young man or woman can prove next to impossible. The Eunice Kennedy Shriver National Institute of Child Health and Human Development recently provided a road map that families should find helpful. Their findings suggest that kids between ages 12 and 15 with Type 1 Diabetes benefitted dramatically from a two-year program (of three to four meetings a year) with parents and a health advisor to discuss shared responsibilities, goals and strategies for solving diabetes management problems that arose. Meeting with a health advisor during regular diabetes clinic visits, researchers reported, helped families better manage the changes that occur as children take on more responsibility for their day-to-day diabetes care.
New Road Map for Families of Teen Diabetics For many parents, coping day-to-day with their teenagers is the most difficult, aggravating and exhausting phase of the child-rearing process. For parents of teens with Type 1 Diabetes, managing the disease and the young man or woman can prove next to impossible. The Eunice Kennedy Shriver National Institute of Child Health and Human Development recently provided a road map that families should find helpful. Their findings suggest that kids between ages 12 and 15 with Type 1 Diabetes benefitted dramatically from a two-year program (of three to four meetings a year) with parents and a health advisor to discuss shared responsibilities, goals and strategies for solving diabetes management problems that arose. Meeting with a health advisor during regular diabetes clinic visits, researchers reported, helped families better manage the changes that occur as children take on more responsibility for their day-to-day diabetes care. Impact of the NYC Soda Ban The announcement of an impending ban in New York City on large, sugary drinks has prompted many people—both inside and outside of the medical profession—to chime in on what, if any, effects this will have on overall health. Obviously, gulping down quarts of soda, energy drinks and sweetened teas a week is not a smart idea. But will shaving a few ounces off this total make a difference? The consensus thus far is that it will—but only a small difference. Obesity is a complex disease, involving a lot of variables. That being said, if the “soda ban” pushes forward the national discussion about the dangers of consuming too much sugar—and overeating in general—it could have a significant impact. Lifestyle changes are often triggered by cultural changes; if the culture of junk-food consumption is altered through publicity and awareness that begins in New York, we may look back on this law as a true game-changer.
Impact of the NYC Soda Ban The announcement of an impending ban in New York City on large, sugary drinks has prompted many people—both inside and outside of the medical profession—to chime in on what, if any, effects this will have on overall health. Obviously, gulping down quarts of soda, energy drinks and sweetened teas a week is not a smart idea. But will shaving a few ounces off this total make a difference? The consensus thus far is that it will—but only a small difference. Obesity is a complex disease, involving a lot of variables. That being said, if the “soda ban” pushes forward the national discussion about the dangers of consuming too much sugar—and overeating in general—it could have a significant impact. Lifestyle changes are often triggered by cultural changes; if the culture of junk-food consumption is altered through publicity and awareness that begins in New York, we may look back on this law as a true game-changer. Genetic Connection to Blindness More than 15 million people around the world suffer from blindness brought on by Primary Angle Closure Glaucoma (PACG). The problem is especially pronounced among Asian populations, which account for about 12 million of these cases. A collaborative international research effort launched in Singapore recently identified three previously unknown genes associated with PACG. The medical community has long suspected the disease to be strongly hereditary, but these findings—published in the journal Nature Genetics—confirm the fact. This opens the door to possibilities of novel treatments, as well as the potential of early identification of people at risk for PACG. “These data are the first critical steps toward a better understanding of the underlying molecular events responsible for this blinding disease,” explains Dr. Janey Wiggs, Professor of Ophthalmology at Harvard Medical School.
Genetic Connection to Blindness More than 15 million people around the world suffer from blindness brought on by Primary Angle Closure Glaucoma (PACG). The problem is especially pronounced among Asian populations, which account for about 12 million of these cases. A collaborative international research effort launched in Singapore recently identified three previously unknown genes associated with PACG. The medical community has long suspected the disease to be strongly hereditary, but these findings—published in the journal Nature Genetics—confirm the fact. This opens the door to possibilities of novel treatments, as well as the potential of early identification of people at risk for PACG. “These data are the first critical steps toward a better understanding of the underlying molecular events responsible for this blinding disease,” explains Dr. Janey Wiggs, Professor of Ophthalmology at Harvard Medical School. New Study on Job Stress When Johnny Paycheck recorded the country hit “Take This Job and Shove It” back in the 1970s, it turns out he was way ahead of his time. Doctors in England recently completed a study that shows workers who feel over-pressured yet powerless run a risk of coronary disease that is 23% greater than those who are content in their work environment. The study covered around 200,000 workers in a wide range of occupations, from civil servants to factory workers. Subjects were asked about the type of work they did, the workload, deadlines and freedom to make decisions.
New Study on Job Stress When Johnny Paycheck recorded the country hit “Take This Job and Shove It” back in the 1970s, it turns out he was way ahead of his time. Doctors in England recently completed a study that shows workers who feel over-pressured yet powerless run a risk of coronary disease that is 23% greater than those who are content in their work environment. The study covered around 200,000 workers in a wide range of occupations, from civil servants to factory workers. Subjects were asked about the type of work they did, the workload, deadlines and freedom to make decisions.





 Editor’s Note: Jim Dunleavy is the Director of Physical Therapy and Rehabilitation for Trinitas Regional Medical Center.
Editor’s Note: Jim Dunleavy is the Director of Physical Therapy and Rehabilitation for Trinitas Regional Medical Center.
 The Ankle Bone’s Connected to the…What? That broken ankle may lead to bigger problems. So say researchers at Texas Tech, who recently established a link between ankle injuries and life-threatening complications, including deep vein thrombosis and pulmonary embolisms. The study suggested that treating physicians should assess patients with ankle fracture for their risk of developing a venous thromboembolic event on an individual basis, and also provide thromboprophylaxis (prevention of thrombosis) for those with an increased risk of developing such complications.
The Ankle Bone’s Connected to the…What? That broken ankle may lead to bigger problems. So say researchers at Texas Tech, who recently established a link between ankle injuries and life-threatening complications, including deep vein thrombosis and pulmonary embolisms. The study suggested that treating physicians should assess patients with ankle fracture for their risk of developing a venous thromboembolic event on an individual basis, and also provide thromboprophylaxis (prevention of thrombosis) for those with an increased risk of developing such complications. Let’s Do (it at) Lunch As a rule, people don’t mind paying the tab to achieve healthy, beautiful skin. Finding the time to make it happen is often the greater obstacle. According to plastic surgeon Dr. Joseph D. Alkon, there are a number of non-invasive, “lunchtime” treatments that can make your skin look and feel its best. “A chemical peel helps those with dry skin, uneven tone, acne, discoloration and/or mild wrinkles,” Dr. Alkon says. “This office-based procedure uses a special liquid to remove the harsh outer layers of skin, while leaving smoother and healthier layers intact. Peels vary from mild to aggressive depending on the skin being treated.” Microdermabrasion also works to remove unhealthy, dry, flaky outer skin, he adds. This procedure uses a gentle tool or wand to remove the outer layers of skin. This leaves behind fresh, healthy skin. Although commonly performed on the face, other body parts can benefit from both chemical peels and microdermabrasion. “A facial is another popular, relaxing and rejuvenating service,” Dr. Alkon says. “It’s often performed by a licensed esthetician, and includes a skin analysis followed by customized exfoliation, extraction, massage, and application of toners, moisturizers, and sunscreens customized to your skin type. A facial can leave the skin clean, clear, hydrated, and rejuvenated.”
Let’s Do (it at) Lunch As a rule, people don’t mind paying the tab to achieve healthy, beautiful skin. Finding the time to make it happen is often the greater obstacle. According to plastic surgeon Dr. Joseph D. Alkon, there are a number of non-invasive, “lunchtime” treatments that can make your skin look and feel its best. “A chemical peel helps those with dry skin, uneven tone, acne, discoloration and/or mild wrinkles,” Dr. Alkon says. “This office-based procedure uses a special liquid to remove the harsh outer layers of skin, while leaving smoother and healthier layers intact. Peels vary from mild to aggressive depending on the skin being treated.” Microdermabrasion also works to remove unhealthy, dry, flaky outer skin, he adds. This procedure uses a gentle tool or wand to remove the outer layers of skin. This leaves behind fresh, healthy skin. Although commonly performed on the face, other body parts can benefit from both chemical peels and microdermabrasion. “A facial is another popular, relaxing and rejuvenating service,” Dr. Alkon says. “It’s often performed by a licensed esthetician, and includes a skin analysis followed by customized exfoliation, extraction, massage, and application of toners, moisturizers, and sunscreens customized to your skin type. A facial can leave the skin clean, clear, hydrated, and rejuvenated.”  New Alzheimer’s Drug May Be on Horizon The medical profession has accepted the fact that there is no “cure” for Alzheimer’s. However, a trial just concluded found that patients who had injections every two weeks of the drug immunoglobulin—made from antibodies in human blood—showed no decline in cognition, memory, daily functioning or mood for a period of three years. Immunoglobulin is normally given to patients who suffer from an immune deficiency, and is extremely costly. If all goes well, however, the drug would be on the market within 10 years. “This is probably the most exciting drug we know about that is currently in the late stages of research,” says Clive Ballard, Director of Research at the Alzheimer’s Society. “We now know it is safe. But the real test will be whether these initial promising results can subsequently be replicated in larger groups.” As life spans increase, the likelihood that a person over the age of 65 will develop some form of dementia is about one in three. Currently, there are only three drugs for Alzheimer’s in the early to moderate stages, and they are effective in some patients but not in others.
New Alzheimer’s Drug May Be on Horizon The medical profession has accepted the fact that there is no “cure” for Alzheimer’s. However, a trial just concluded found that patients who had injections every two weeks of the drug immunoglobulin—made from antibodies in human blood—showed no decline in cognition, memory, daily functioning or mood for a period of three years. Immunoglobulin is normally given to patients who suffer from an immune deficiency, and is extremely costly. If all goes well, however, the drug would be on the market within 10 years. “This is probably the most exciting drug we know about that is currently in the late stages of research,” says Clive Ballard, Director of Research at the Alzheimer’s Society. “We now know it is safe. But the real test will be whether these initial promising results can subsequently be replicated in larger groups.” As life spans increase, the likelihood that a person over the age of 65 will develop some form of dementia is about one in three. Currently, there are only three drugs for Alzheimer’s in the early to moderate stages, and they are effective in some patients but not in others. Smile and Say “Aaaaaah” Do you experience nausea, bloating, heartburn, constipation, or a feeling of fullness? These may be symptoms of a motility disorder, such as gastroparesis and chronic constipation. Gastropathy is a common condition in long standing diabetic people, especially if not well controlled. People with gastropathy can suffer from postprandial indigestion, abdominal discomfort, nausea, and vomiting. Fortunately, the guesswork has been removed from diagnosis of these conditions thanks to the SmartPill, a wireless motility capsule procedure. “The SmartPill capsule travels through your GI tract, collects data, which is then recorded for your doctor to evaluate,” explains Samiappan Muthusamy M.D. of the Center for Digestive Diseases (cddnj.com), which offers this state-of-the art procedure. According to Dr. Muthusamy, the SmartPill can also diagnose Diffuse Colonic Dysfunction (aka lack of colon motility), an extremely serious condition that can present as constipation. Of course, causes such as a poor diet, lack of fluids, sluggish thyroid, colon cancer and constipating medications are ruled out first. “In modern medicine,” adds Dr. Muthusamy, “living with gastropathy and constipation is a thing of the past. They are treatable.”
Smile and Say “Aaaaaah” Do you experience nausea, bloating, heartburn, constipation, or a feeling of fullness? These may be symptoms of a motility disorder, such as gastroparesis and chronic constipation. Gastropathy is a common condition in long standing diabetic people, especially if not well controlled. People with gastropathy can suffer from postprandial indigestion, abdominal discomfort, nausea, and vomiting. Fortunately, the guesswork has been removed from diagnosis of these conditions thanks to the SmartPill, a wireless motility capsule procedure. “The SmartPill capsule travels through your GI tract, collects data, which is then recorded for your doctor to evaluate,” explains Samiappan Muthusamy M.D. of the Center for Digestive Diseases (cddnj.com), which offers this state-of-the art procedure. According to Dr. Muthusamy, the SmartPill can also diagnose Diffuse Colonic Dysfunction (aka lack of colon motility), an extremely serious condition that can present as constipation. Of course, causes such as a poor diet, lack of fluids, sluggish thyroid, colon cancer and constipating medications are ruled out first. “In modern medicine,” adds Dr. Muthusamy, “living with gastropathy and constipation is a thing of the past. They are treatable.” UGNJ Strikes Gold The Urology Group of New Jersey (UGNJ) recently earned The Joint Commission’s Gold Seal of Approval for its continuous standards of healthcare quality and safety in ambulatory care. By receiving this accreditation award, UGNJ is now the only Urology physician practice in the nation to achieve this status. Recognition followed a rigorous unannounced on-site survey of all 12 UGNJ offices in March 2012 by a team of expert surveyors, who evaluated the group’s standards of care specific to the needs of patients—including prevention of infection, leadership and medication management. “Achieving accreditation from The Joint Commission is a team effort that will bring confidence to our patients and give us a framework to provide the best care possible,” says Dr. Alan Krieger, UGNJ’s President.
UGNJ Strikes Gold The Urology Group of New Jersey (UGNJ) recently earned The Joint Commission’s Gold Seal of Approval for its continuous standards of healthcare quality and safety in ambulatory care. By receiving this accreditation award, UGNJ is now the only Urology physician practice in the nation to achieve this status. Recognition followed a rigorous unannounced on-site survey of all 12 UGNJ offices in March 2012 by a team of expert surveyors, who evaluated the group’s standards of care specific to the needs of patients—including prevention of infection, leadership and medication management. “Achieving accreditation from The Joint Commission is a team effort that will bring confidence to our patients and give us a framework to provide the best care possible,” says Dr. Alan Krieger, UGNJ’s President. Mapping Menopause A study published in July by the Endocrine Society suggests that the primary barrier to women receiving hormone therapy to treat menopausal symptoms is patients’ fears about the risks, and their unwillingness to discuss the option. What is interesting about this study is that it was conducted with internal medicine, family practice and OB/GYN physicians—and not patients. “Nearly every physician participating in the survey said menopausal symptoms have a negative impact on quality of life,” says William F. Young, Jr., MD, president of The Endocrine Society. “It’s important for a woman to know what hormonal and non-hormonal treatment options may be best for them to provide symptom relief.” To that end, the Society has created what it calls the Menopause Map, an online interactive tool that guides a woman through the different options available to get relief from her symptoms. The map uses a series of prompting questions about those symptoms and her personal health history, and also has links to questionnaires that help assess current risk for breast cancer, heart disease, and stroke. The tool weighs hormonal and non-hormonal therapies against the risks based on individual symptoms and medical history. The url is hormone.org/MenopauseMap.
Mapping Menopause A study published in July by the Endocrine Society suggests that the primary barrier to women receiving hormone therapy to treat menopausal symptoms is patients’ fears about the risks, and their unwillingness to discuss the option. What is interesting about this study is that it was conducted with internal medicine, family practice and OB/GYN physicians—and not patients. “Nearly every physician participating in the survey said menopausal symptoms have a negative impact on quality of life,” says William F. Young, Jr., MD, president of The Endocrine Society. “It’s important for a woman to know what hormonal and non-hormonal treatment options may be best for them to provide symptom relief.” To that end, the Society has created what it calls the Menopause Map, an online interactive tool that guides a woman through the different options available to get relief from her symptoms. The map uses a series of prompting questions about those symptoms and her personal health history, and also has links to questionnaires that help assess current risk for breast cancer, heart disease, and stroke. The tool weighs hormonal and non-hormonal therapies against the risks based on individual symptoms and medical history. The url is hormone.org/MenopauseMap.
 beach the following summer resulted in the wound festering still further into a situation so serious that it could easily have become limb-threatening. Out of sheer frustration and in near panic, Schroeding resorted to doing his own research on the Internet and identified two out-of-state hospitals with highly renowned wound care centers: Johns Hopkins in Baltimore and Trinitas Regional Medical Center in Elizabeth. The Hopkins website cited a 60-70% heal rate, whereas Trinitas claimed more than 90% overall. That made the choice easy.
beach the following summer resulted in the wound festering still further into a situation so serious that it could easily have become limb-threatening. Out of sheer frustration and in near panic, Schroeding resorted to doing his own research on the Internet and identified two out-of-state hospitals with highly renowned wound care centers: Johns Hopkins in Baltimore and Trinitas Regional Medical Center in Elizabeth. The Hopkins website cited a 60-70% heal rate, whereas Trinitas claimed more than 90% overall. That made the choice easy.
 Don’t Walk Sign Are you a sleepwalker? If so, you’re definitely not alone. New research by the Stanford University School of Medicine found that somnambulism is far more prevalent than previous studies suggested. About 3.6 percent of American adults are prone to nocturnal wandering. That translates to 8.4 million. The same research suggests that sleepwalking is linked to anxiety and depression. A subject of humor and silliness in popular culture, this disorder can actually have serious consequences. Sleepwalkers have been known to injure themselves and others. They are also prone to psychosocial disorders. The Trinitas Sleep Disorders Center deals with sleepwalking and other problems every day. For information call 908-994-8694.
Don’t Walk Sign Are you a sleepwalker? If so, you’re definitely not alone. New research by the Stanford University School of Medicine found that somnambulism is far more prevalent than previous studies suggested. About 3.6 percent of American adults are prone to nocturnal wandering. That translates to 8.4 million. The same research suggests that sleepwalking is linked to anxiety and depression. A subject of humor and silliness in popular culture, this disorder can actually have serious consequences. Sleepwalkers have been known to injure themselves and others. They are also prone to psychosocial disorders. The Trinitas Sleep Disorders Center deals with sleepwalking and other problems every day. For information call 908-994-8694.

 Another Link Between TV & Obesity From the “Wait, Didn’t We Know that Already?” department comes the news that kids who watch a lot of TV have poorer overall diets than kids whose exposure to television is limited. “The more TV you watch, the less likely you were to eat fruits and vegetables every day, and the more likely you were to eat things like candy and soda, eat at a fast-food restaurant and even skip breakfast,” says study author Leah Lipsky of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The research doesn’t prove that TV watching influences what kids eat, but strongly suggests a link between TV, snacking and a lack of exercise. Add questionable parenting to the mix and you have yet another contributing factor to America’s epidemic of childhood obesity. The average age of the children in the study was 13.
Another Link Between TV & Obesity From the “Wait, Didn’t We Know that Already?” department comes the news that kids who watch a lot of TV have poorer overall diets than kids whose exposure to television is limited. “The more TV you watch, the less likely you were to eat fruits and vegetables every day, and the more likely you were to eat things like candy and soda, eat at a fast-food restaurant and even skip breakfast,” says study author Leah Lipsky of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The research doesn’t prove that TV watching influences what kids eat, but strongly suggests a link between TV, snacking and a lack of exercise. Add questionable parenting to the mix and you have yet another contributing factor to America’s epidemic of childhood obesity. The average age of the children in the study was 13.
 Smoking While Pregnant: Are Friends Actually Foes? Most people are aware that smoking and pregnancy don’t mix. Yet expectant mothers continue to puff away, or live in smoking environments. A recent study published in the journal Addictive Behaviors looked at some of the reasons this situation persists. It was no shock to find that nearly half of pregnant women who smoke had a partner who also smoked. It was a surprise, however, to find that women who had close friends that smoke were far more likely to smoke themselves. In fact, the influence of friends was actually higher than the influence of family members. The study, conducted by researchers at SUNY Buffalo from 2006 to 2011, will continue, and focus on generating data on the children of pregnant smokers.
Smoking While Pregnant: Are Friends Actually Foes? Most people are aware that smoking and pregnancy don’t mix. Yet expectant mothers continue to puff away, or live in smoking environments. A recent study published in the journal Addictive Behaviors looked at some of the reasons this situation persists. It was no shock to find that nearly half of pregnant women who smoke had a partner who also smoked. It was a surprise, however, to find that women who had close friends that smoke were far more likely to smoke themselves. In fact, the influence of friends was actually higher than the influence of family members. The study, conducted by researchers at SUNY Buffalo from 2006 to 2011, will continue, and focus on generating data on the children of pregnant smokers. Good News on Concussions If you happen to be a hockey fan, you know that NHL superstar Sidney Crosby nearly lost his entire season to a concussion. What finally helped him get back on the ice was the diagnosis and treatment of a soft-tissue neck injury that accompanied the concussion. This was no surprise to the doctors at the MMTR Health Clinic in Guelph, Ontario, which has been treating hockey concussions for years. They have found that many symptoms attributed to the lingering effects of a concussion actually correspond to specific neck muscles damaged at the time of the original injury. Once treatment is individualized and the muscles repaired, patients experience speedy postconcussive recoveries.
Good News on Concussions If you happen to be a hockey fan, you know that NHL superstar Sidney Crosby nearly lost his entire season to a concussion. What finally helped him get back on the ice was the diagnosis and treatment of a soft-tissue neck injury that accompanied the concussion. This was no surprise to the doctors at the MMTR Health Clinic in Guelph, Ontario, which has been treating hockey concussions for years. They have found that many symptoms attributed to the lingering effects of a concussion actually correspond to specific neck muscles damaged at the time of the original injury. Once treatment is individualized and the muscles repaired, patients experience speedy postconcussive recoveries. a Body Mass Index (BMI) of 18.5 or more. A media storm ensued, with critics of the law saying the government should aim its efforts on health as opposed to weight. Indeed, some models now disqualified are naturally skinny and completely healthy. Should they be prevented from earning a living without knowing whether they are actually unhealthy in some way? The Israeli government points to statistics that show 1 in 50 teenage girls suffers from an eating disorder, and stands by its position.
a Body Mass Index (BMI) of 18.5 or more. A media storm ensued, with critics of the law saying the government should aim its efforts on health as opposed to weight. Indeed, some models now disqualified are naturally skinny and completely healthy. Should they be prevented from earning a living without knowing whether they are actually unhealthy in some way? The Israeli government points to statistics that show 1 in 50 teenage girls suffers from an eating disorder, and stands by its position. Is There an Autism Epidemic? A March study released by the Centers for Disease Control and Prevention estimates that 1 in 88 children born in the U.S. suffers from a disorder on the autism spectrum. The last study estimated the ratio to be 1 in 110 and one done in 2002 suggests that the number of autistic children has doubled since then to around one million. Does this mean there is an “epidemic” of autism? Most doctors and researchers believe this is not the case. Instead, the numbers reflect better diagnostic screening tools and earlier detection. There is no “test” for autism, such as a blood test; it is detected through observing behavior of children typically around the age of eight. “One thing the data tells us with certainty,” says CDC Director Dr. Thomas Frieden, “is there are many children and families who need help.”
Is There an Autism Epidemic? A March study released by the Centers for Disease Control and Prevention estimates that 1 in 88 children born in the U.S. suffers from a disorder on the autism spectrum. The last study estimated the ratio to be 1 in 110 and one done in 2002 suggests that the number of autistic children has doubled since then to around one million. Does this mean there is an “epidemic” of autism? Most doctors and researchers believe this is not the case. Instead, the numbers reflect better diagnostic screening tools and earlier detection. There is no “test” for autism, such as a blood test; it is detected through observing behavior of children typically around the age of eight. “One thing the data tells us with certainty,” says CDC Director Dr. Thomas Frieden, “is there are many children and families who need help.”

 You may have heard some encouraging news over the holidays about the fight against HIV/AIDS. The United Nations announced that both AIDS-related deaths and new HIV infections have dropped to their lowest levels since the peak of the epidemic in the 1990s. Worldwide, new infections have dropped 21% since 1997 and deaths were down 21% since 2005. Researchers credit a combination of things for the dramatic improvements, including scientific breakthroughs, access to treatment, better political leadership and social change. The UN report also noted that HIV-infected individuals are also living longer.
You may have heard some encouraging news over the holidays about the fight against HIV/AIDS. The United Nations announced that both AIDS-related deaths and new HIV infections have dropped to their lowest levels since the peak of the epidemic in the 1990s. Worldwide, new infections have dropped 21% since 1997 and deaths were down 21% since 2005. Researchers credit a combination of things for the dramatic improvements, including scientific breakthroughs, access to treatment, better political leadership and social change. The UN report also noted that HIV-infected individuals are also living longer. abdominal cramping underscores the importance of catching colon cancer in its early stages. This individual, who was literally surrounded by doctors every day, put off a visit to his GP until the condition became unbearable. When he finally had it checked out, he was diagnosed with metastatic inoperable carcinoma of the colon. Colon cancer is the third leading cause of cancer-related death for both men and women. Yet it is 95 percent curable if diagnosed before symptoms arise. Most colorectal cancer begins as a non-cancerous (benign) adenoma or polyp (abnormal growth) that develops on the lining of the colon or rectum. Polyps can be removed to significantly reduce the risk of cancer.
abdominal cramping underscores the importance of catching colon cancer in its early stages. This individual, who was literally surrounded by doctors every day, put off a visit to his GP until the condition became unbearable. When he finally had it checked out, he was diagnosed with metastatic inoperable carcinoma of the colon. Colon cancer is the third leading cause of cancer-related death for both men and women. Yet it is 95 percent curable if diagnosed before symptoms arise. Most colorectal cancer begins as a non-cancerous (benign) adenoma or polyp (abnormal growth) that develops on the lining of the colon or rectum. Polyps can be removed to significantly reduce the risk of cancer. E-Shoppers Under the Influence One of the most unusual trends to emerge this past holiday season was a sharp rise in “drunk shopping.” Drunk shopping is exactly what it sounds like. People have a couple of drinks, go online, and start buying things they normally wouldn’t. E-tailers know this is happening. They can tell when someone orders 10 of something instead of one—they have impatiently clicked the BUY button too many times. Another sign is when shoppers botch selections from a drop-down menu, such as which state they live in.
E-Shoppers Under the Influence One of the most unusual trends to emerge this past holiday season was a sharp rise in “drunk shopping.” Drunk shopping is exactly what it sounds like. People have a couple of drinks, go online, and start buying things they normally wouldn’t. E-tailers know this is happening. They can tell when someone orders 10 of something instead of one—they have impatiently clicked the BUY button too many times. Another sign is when shoppers botch selections from a drop-down menu, such as which state they live in. risk of miscarriage, underweight birth, or diminished IQ for her baby. Doctors know to treat severe cases with hormone medication, but there is a growing debate about how to handle milder “gray-area” cases. Roughly a quarter of pregnant women receive a thyroid blood test whether they have symptoms or not. Testing lab Quest Diagnostics recently reported that about 15% of the expectant mothers it tested showed signs of an underactive thyroid, which surprised many. An underactive thyroid (aka hypothyroidism) slows body functions, causing such problems as fatigue, weight gain and depression.
risk of miscarriage, underweight birth, or diminished IQ for her baby. Doctors know to treat severe cases with hormone medication, but there is a growing debate about how to handle milder “gray-area” cases. Roughly a quarter of pregnant women receive a thyroid blood test whether they have symptoms or not. Testing lab Quest Diagnostics recently reported that about 15% of the expectant mothers it tested showed signs of an underactive thyroid, which surprised many. An underactive thyroid (aka hypothyroidism) slows body functions, causing such problems as fatigue, weight gain and depression. to protect themselves by staying slim and active, focusing on healthful, natural foods, and avoiding the disease-causing foods common in the standard American diet. According to Dr. Joel Fuhrman, author of Super Immunity, the keys to a cancer-resisting diet include getting your folic acid from green vegetables (as opposed to the synthetic type contained in multivitamins and prenatal vitamins); taking a daily dose of ground flaxseed (which contains estrogen-blocking lignans); eating your GOMBBS (greens, onions, mushrooms, beans, berries and seeds); minimizing the consumption of meat, fish and dairy products, and avoiding white flour and sugars.
to protect themselves by staying slim and active, focusing on healthful, natural foods, and avoiding the disease-causing foods common in the standard American diet. According to Dr. Joel Fuhrman, author of Super Immunity, the keys to a cancer-resisting diet include getting your folic acid from green vegetables (as opposed to the synthetic type contained in multivitamins and prenatal vitamins); taking a daily dose of ground flaxseed (which contains estrogen-blocking lignans); eating your GOMBBS (greens, onions, mushrooms, beans, berries and seeds); minimizing the consumption of meat, fish and dairy products, and avoiding white flour and sugars.
 Calderon, Ed. D—the museum’s Director of Science and curator of Generation Fit—gave EDGE a tantalizing sneak peek. Calderon calls it an exploratory space, and that it is. But here’s the clever part—as kids explore the interactive exhibits, lessons of healthy eating, the benefits of exercise and a profound awareness of their own bodies start to sink in.
Calderon, Ed. D—the museum’s Director of Science and curator of Generation Fit—gave EDGE a tantalizing sneak peek. Calderon calls it an exploratory space, and that it is. But here’s the clever part—as kids explore the interactive exhibits, lessons of healthy eating, the benefits of exercise and a profound awareness of their own bodies start to sink in. interactive display provides feedback on whether the selected meal is sufficiently balanced. It also provides alternative food choices. As you work your way around the exhibit hall, you’ll encounter the Label Decoder, Sugar Detective, Dollars and Scents, Know Your BMI, Exertainment and FIT Center (FIT is an acronym for frequency, intensity & time). You can probably make an educated guess at what each offers, and you’d be right. The key thing here is that Calderon (left) has seen to it that each section over-delivers. Two good things to know about Generation Fit. First, to avoid the chaos and disorder that sometimes diminish other interactive children’s exhibits, the Newark Museum will probably be time-ticketing the exhibit. This is a great idea. Call ahead to get details on this. Second, the crowded times for Generation Fit will probably be between noon and 2:00 pm. Plan accordingly.
interactive display provides feedback on whether the selected meal is sufficiently balanced. It also provides alternative food choices. As you work your way around the exhibit hall, you’ll encounter the Label Decoder, Sugar Detective, Dollars and Scents, Know Your BMI, Exertainment and FIT Center (FIT is an acronym for frequency, intensity & time). You can probably make an educated guess at what each offers, and you’d be right. The key thing here is that Calderon (left) has seen to it that each section over-delivers. Two good things to know about Generation Fit. First, to avoid the chaos and disorder that sometimes diminish other interactive children’s exhibits, the Newark Museum will probably be time-ticketing the exhibit. This is a great idea. Call ahead to get details on this. Second, the crowded times for Generation Fit will probably be between noon and 2:00 pm. Plan accordingly.
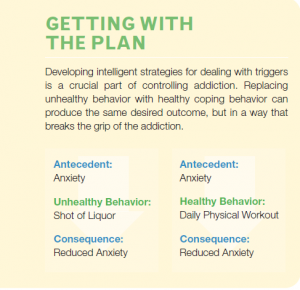 Goddard: The greater our ability to identify a trigger, the stronger we become at overcoming an addiction. Trigger awareness can help us to substitute a behavior that does not injure our health or quality of life. When we can identify our triggers it is possible to stop the negative action before it takes us over. Writing down triggers can be a first step in overcoming addictions. Sometimes we are able to overcome an addiction on our own, but sometimes it is critical to get help from a therapist, clinic or professionals that specialize in addiction.
Goddard: The greater our ability to identify a trigger, the stronger we become at overcoming an addiction. Trigger awareness can help us to substitute a behavior that does not injure our health or quality of life. When we can identify our triggers it is possible to stop the negative action before it takes us over. Writing down triggers can be a first step in overcoming addictions. Sometimes we are able to overcome an addiction on our own, but sometimes it is critical to get help from a therapist, clinic or professionals that specialize in addiction.