With each 9-1-1 call, two award-winning Trinitas teams spring into action.
Terror. Pain. Confusion. A swirl of sounds and people. The fear that this might be a one-way trip. This is the part of a cardiac emergency you don’t see on TV medical dramas. Yet it is in these first moments when help arrives that difference-making action begins. The target window of time during which an individual in this situation needs to receive emergency care is 90 minutes—so says the American Heart Association. Which is why the right call is a 9-1-1 call. Indeed, according to Gerard “Rod” Muench, Trinitas Regional Medical Center  Administrative Director of the Emergency and Emergency Medical Services Departments, a good chunk of that critical window can be wasted by driving that individual to the hospital in a personal vehicle. Dialing 9-1-1 initiates a System of Care that makes the most of those precious minutes.
Administrative Director of the Emergency and Emergency Medical Services Departments, a good chunk of that critical window can be wasted by driving that individual to the hospital in a personal vehicle. Dialing 9-1-1 initiates a System of Care that makes the most of those precious minutes.
Trinitas has been the recipient of Mission: Lifeline awards from the American Heart Association in each of the last four years. The departments receiving this honor are under the director- ship of Muench and Kathleen Azzarello, head of Cardiovascular Services—two professionals who excel at administering critical emergency-treatment response. Muench’s team is focused on saving the lives of severely distressed cardiac (and other) patients by streamlining the trip of EMS personnel from point of contact to the Emergency Department at Trinitas. Azzarello’s team, which includes the cardiac catheterization lab, is at the receiving end when the ambulance arrives with patients in cardiac distress.
Muench and his team deliver approximately 1,000 patients each year to Azzarello and her staff. On average, their coordinated care probably saves 50 patients a year—about one a week—whose extreme coronary distress would have resulted in death under almost any other scenario.
The Three C’s
The common goal of emergency System of Care protocols can be defined by three important C’s: Cooperation, Collaboration and Communication. The goal of the EMS team is to administer treatment at the very first moment that the EMTs make contact with the patient. Trinitas pre-hospital personnel is trained in procedures such as administering CPR, providing medication, inserting an IV, and transmitting an EKG to the hospital prior to the patient’s arrival. Once delivered to the Emergency Department, no time is wasted in turning over those in need of immediate cardiac care to the Cardiovascular Services Department.
at the very first moment that the EMTs make contact with the patient. Trinitas pre-hospital personnel is trained in procedures such as administering CPR, providing medication, inserting an IV, and transmitting an EKG to the hospital prior to the patient’s arrival. Once delivered to the Emergency Department, no time is wasted in turning over those in need of immediate cardiac care to the Cardiovascular Services Department.
The overall success of response to cardiac emergencies starts with expediting what used to be called “door-to-needle” time. The clock starts ticking at the point of first medical contact—in the home, in the car, at work, or on the phone with a 911 dispatcher—and doesn’t stop until a patient is transported by an emergency vehicle to the catheterization lab or cardiovascular department, where life-saving treatment can be initiated before time runs out. At Trinitas, first contact typically goes through the hospital’s Mobile Intensive Care Unit. The MICU operates in coordination with the Elizabeth Fire Department, which initiates on-site stabilization and treatment.
Everyone trained and supervised by Rod Muench appreciates that every minute matters when it comes to coronary patient outcomes, making the MICU an “Emergency Dept. on wheels.” He has been at Trinitas for 11 years, previously served as ED/EMS Administrator, and is often described as a paramedic educator. He has developed and implemented a thorough regimen for the hospital’s staff of EMTs, including a first-contact philosophy.
“Learning how to communicate with the patient is key,” Muench explains. “Good people skills are essential to a good emergency medical technician.”
The need to combine empathy with speed and accuracy is echoed by Kathleen Azzarello and her team, which deals with extreme pressure  situations on a round-the-clock basis. In assembling that team, she looks for individuals who are “a bit of an adrenaline junkie,” adding that they need to stay calm under fire and also appreciate the ultimate rewards of being a critical caregiver. What is her reward?
situations on a round-the-clock basis. In assembling that team, she looks for individuals who are “a bit of an adrenaline junkie,” adding that they need to stay calm under fire and also appreciate the ultimate rewards of being a critical caregiver. What is her reward?
“It’s an amazing privilege to watch a cardiac patient go from near death upon arrival to wanting to leave the hospital as soon as treatment has been administered.”
Needless to say, COVID-19 has complicated the work of everyone involved in emergency care. It has also created a growing number of post-COVID coronary infections, a story that was under-reported in 2020. Given the added stress of the pandemic, Azzarello and Muench are understandably proud of the Mission: Lifeline recognition their teams received in 2020—the Gold Plus award to the ED/EMS departments and the Gold Mission: Lifeline for ST Elevation Myocardial Infarction (STEMI) Receiving Department. Neither, however, is quick to take personal credit.
STEMI
According to the CDC, even in the pandemic year of 2020, heart disease was the number-one cause of death in the United States. A quarter-million people fall victim to the most fatal type of heart attack —ST Elevation Myocardial Infarction, or STEMI—which blocks blood flow to the heart. These extreme cases are prime examples of the difference that a 9-1-1 call to Trinitas can make.
—ST Elevation Myocardial Infarction, or STEMI—which blocks blood flow to the heart. These extreme cases are prime examples of the difference that a 9-1-1 call to Trinitas can make.
“I am only doing so well,” Muench points out, “because my staff at Trinitas is a unique breed of highly skilled and motivated people who make my job easier.”
“I am supported by a staff of passionate, humble and unspoiled individuals from diverse backgrounds,” adds Azzarello. “We have become a family that is willing to walk that extra mile to help a patient in need.”



 “Almost all urologists agree that PSA testing benefits far more people than it hurts,” says Andrew Bernstein, MD, adding that the AUA and USPSTF will eventually meet somewhere in the middle. “It is just a blood test. Doctors and patients together make the decision on what to do about the results. In years prior, it was a reflex to proceed with further biopsy work, surgery, or aggressive treatment. We know that is not necessarily mandatory now, but the cost of a blood test is far less than the cost of treating a disease after it has spread.”
“Almost all urologists agree that PSA testing benefits far more people than it hurts,” says Andrew Bernstein, MD, adding that the AUA and USPSTF will eventually meet somewhere in the middle. “It is just a blood test. Doctors and patients together make the decision on what to do about the results. In years prior, it was a reflex to proceed with further biopsy work, surgery, or aggressive treatment. We know that is not necessarily mandatory now, but the cost of a blood test is far less than the cost of treating a disease after it has spread.”
 The Center features state of the art operating rooms offering comprehensive outpatient surgical procedures including plastic surgery, laparoscopic gynecological procedures, gallbladder surgery, hernia repair, orthopedic, vascular, podiatric, and pain management surgeries as well as cutting edge hemorrhoid surgery. Andrea Zimmern, MD, Colorectal Surgeon at Trinitas, is the first surgeon in Union County to carry out Transanal Hemorrhoidal Dearterialization (THD) procedures at the Center. “The groundbreaking THD procedure is virtually painless,” Dr. Zimmern says. “We tie off all the blood vessels that feed the hemorrhoid, and work in an area of the anal canal that has no pain sensory innervation. It’s a drastic, positive change from traditional surgery—patients are back to normal activities usually in less than a week. THD changes the game because we’ve removed the painful discomfort while minimizing recovery time. That’s an amazing advancement when you consider what hemorrhoid surgery used to mean.”
The Center features state of the art operating rooms offering comprehensive outpatient surgical procedures including plastic surgery, laparoscopic gynecological procedures, gallbladder surgery, hernia repair, orthopedic, vascular, podiatric, and pain management surgeries as well as cutting edge hemorrhoid surgery. Andrea Zimmern, MD, Colorectal Surgeon at Trinitas, is the first surgeon in Union County to carry out Transanal Hemorrhoidal Dearterialization (THD) procedures at the Center. “The groundbreaking THD procedure is virtually painless,” Dr. Zimmern says. “We tie off all the blood vessels that feed the hemorrhoid, and work in an area of the anal canal that has no pain sensory innervation. It’s a drastic, positive change from traditional surgery—patients are back to normal activities usually in less than a week. THD changes the game because we’ve removed the painful discomfort while minimizing recovery time. That’s an amazing advancement when you consider what hemorrhoid surgery used to mean.” The Center opened for business in March and will help Trinitas handle a growing demand for same-day surgery. From 2012 to 2013, the hospital experienced a rise of more than 15 percent in these types of procedures, and expects 10 to 15 percent growth in this category to remain steady for several years. About 45 percent of the surgeries performed at Trinitas are already of the outpatient variety.
The Center opened for business in March and will help Trinitas handle a growing demand for same-day surgery. From 2012 to 2013, the hospital experienced a rise of more than 15 percent in these types of procedures, and expects 10 to 15 percent growth in this category to remain steady for several years. About 45 percent of the surgeries performed at Trinitas are already of the outpatient variety.
 Happy Days
Happy Days Patient, Heal Thyself
Patient, Heal Thyself Crisp Reminder
Crisp Reminder
 Where There’s Smoke…
Where There’s Smoke… The Wrong Kind of Tweeting
The Wrong Kind of Tweeting
 Going Deep
Going Deep
 In the Blink of an Eye
In the Blink of an Eye Eating Away the Blues
Eating Away the Blues 16 Going on 17
16 Going on 17
 Nuts to You
Nuts to You
 Vacation Souvenir
Vacation Souvenir
 Autism Breakthrough at Yale
Autism Breakthrough at Yale


 “The visualization [using robotic equipment] is far beyond anything we’ve had previously,” Dr. Zimmern says. “With robotics, we can perform surgeries that used to be impossible even via laparoscopy. We recently treated a patient who came to us with an abdominal tumor that took up his entire pelvis. The patient was also suffering from obesity, which made his case especially complicated. Even with laparoscopy, we wouldn’t have been able to remove the cancer without giving the patient a permanent colostomy. But the precision of our robotic equipment allowed us to do just that. So we’re learning there are particular instances and cases where the ability to carry out robotics-assisted surgery isn’t just advantageous—it’s really the ideal.”
“The visualization [using robotic equipment] is far beyond anything we’ve had previously,” Dr. Zimmern says. “With robotics, we can perform surgeries that used to be impossible even via laparoscopy. We recently treated a patient who came to us with an abdominal tumor that took up his entire pelvis. The patient was also suffering from obesity, which made his case especially complicated. Even with laparoscopy, we wouldn’t have been able to remove the cancer without giving the patient a permanent colostomy. But the precision of our robotic equipment allowed us to do just that. So we’re learning there are particular instances and cases where the ability to carry out robotics-assisted surgery isn’t just advantageous—it’s really the ideal.”



 Do you have a hot topic for Dr. D’Angelo and his Trinitas ER team?
Do you have a hot topic for Dr. D’Angelo and his Trinitas ER team?

 Angela reminds her fellow patients to never stop asking questions or learning about their own treatments. She encourages them to pay attention to their bodies and listen for cues, reminding them that nurses and doctors can only do so much; it’s up to the patients to communicate how they’re feeling and responding.
Angela reminds her fellow patients to never stop asking questions or learning about their own treatments. She encourages them to pay attention to their bodies and listen for cues, reminding them that nurses and doctors can only do so much; it’s up to the patients to communicate how they’re feeling and responding. 

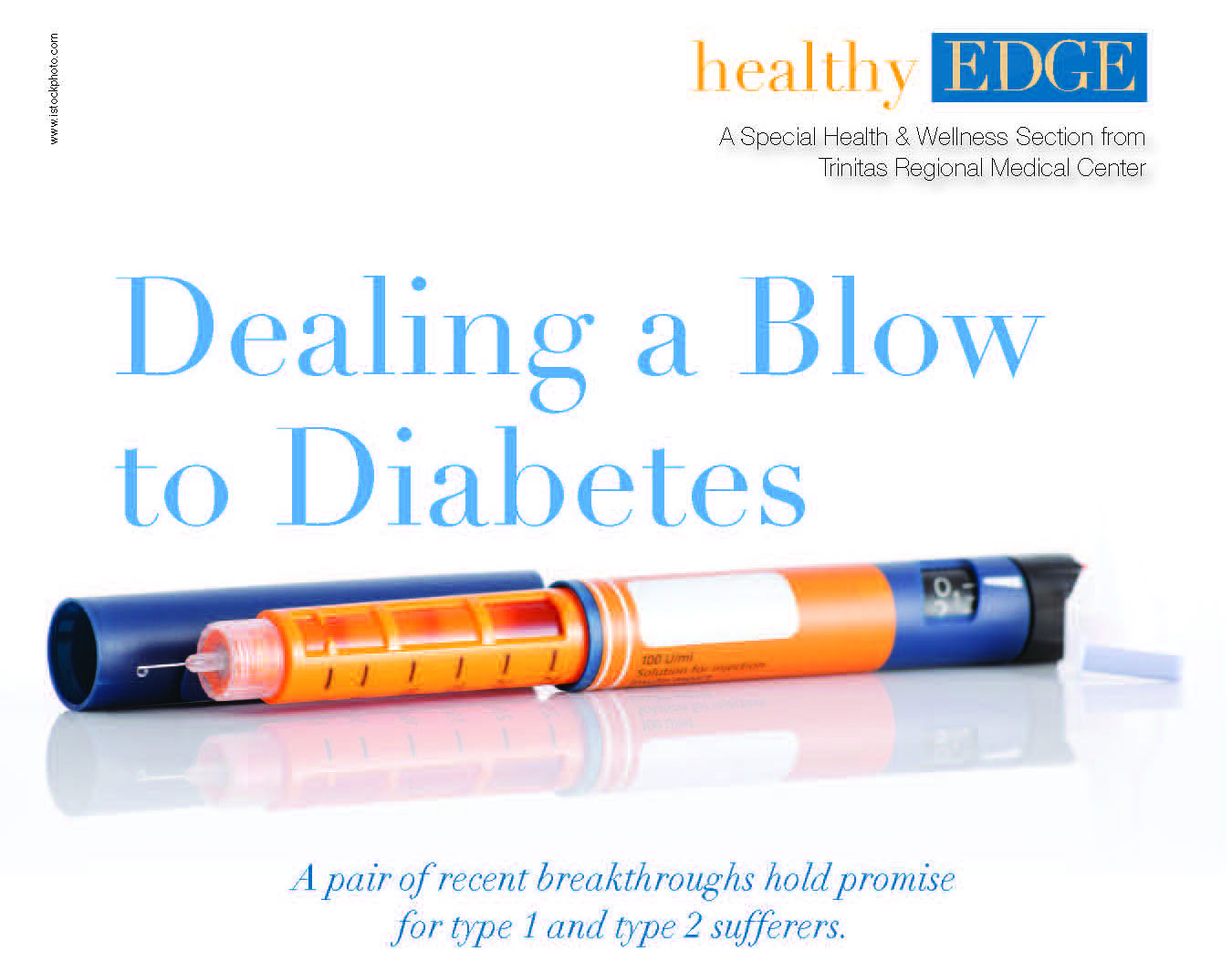
 If you’ve just been diagnosed, or if you’ve been living with diabetes, quality medical care, encouragement and education can make a difference in your daily life.
If you’ve just been diagnosed, or if you’ve been living with diabetes, quality medical care, encouragement and education can make a difference in your daily life.

 Prepare for Takeoff
Prepare for Takeoff 

 Extensive touring and physical wear and tear on Testa over the years resulted in a hip condition that took him off his feet earlier this year. A born performer, Testa knew he couldn’t take chances with anything other than the best care and technology when it came to receiving an artificial hip—a critical joint for someone who needs to command the stage for a living. After researching hip replacement procedures, Testa decided to seek out a facility that uses the Hana Orthopedic Table (right) in its OR. The Hana Table has transformed how hip replacement surgeries are carried out: patient positioning via the table means the surgery can be minimally invasive, less painful, and with much faster recovery time. It all adds up to a vastly improved experience compared to hip replacements of even the recent past. A friend who had recently undergone surgery of his own recommended that Testa—who lives in Jackson Township—look into the work being done at Trinitas, which uses the Hana Table in its OR. After speaking to another friend, Nadine Brechner, Chief Development Officer and Vice President of the Trinitas Health Foundation, Testa chose Trinitas even though Elizabeth is 50-plus miles north of his home.
Extensive touring and physical wear and tear on Testa over the years resulted in a hip condition that took him off his feet earlier this year. A born performer, Testa knew he couldn’t take chances with anything other than the best care and technology when it came to receiving an artificial hip—a critical joint for someone who needs to command the stage for a living. After researching hip replacement procedures, Testa decided to seek out a facility that uses the Hana Orthopedic Table (right) in its OR. The Hana Table has transformed how hip replacement surgeries are carried out: patient positioning via the table means the surgery can be minimally invasive, less painful, and with much faster recovery time. It all adds up to a vastly improved experience compared to hip replacements of even the recent past. A friend who had recently undergone surgery of his own recommended that Testa—who lives in Jackson Township—look into the work being done at Trinitas, which uses the Hana Table in its OR. After speaking to another friend, Nadine Brechner, Chief Development Officer and Vice President of the Trinitas Health Foundation, Testa chose Trinitas even though Elizabeth is 50-plus miles north of his home. 

 Also unprecedented in 2020 was the surge in interest among young New Jerseyans in entering the healthcare field—specifically nursing—at a time when there was no small amount of risk accompanying that decision.
Also unprecedented in 2020 was the surge in interest among young New Jerseyans in entering the healthcare field—specifically nursing—at a time when there was no small amount of risk accompanying that decision.  “I wish I could take every single one of our applicants,” she says, noting that some will have to be waitlisted. “It’s a balancing act, meeting the New Jersey Board of Nursing demand for more licensed nurses while adhering to state-mandated health protocols in our classrooms. We also have to bear in mind the guidelines required by the New Jersey Office of the Secretary of Higher Education.”
“I wish I could take every single one of our applicants,” she says, noting that some will have to be waitlisted. “It’s a balancing act, meeting the New Jersey Board of Nursing demand for more licensed nurses while adhering to state-mandated health protocols in our classrooms. We also have to bear in mind the guidelines required by the New Jersey Office of the Secretary of Higher Education.” 


 Where There’s Vapor…
Where There’s Vapor…
 In Sickness and In Health
In Sickness and In Health
 The Skinny On Oxytocin
The Skinny On Oxytocin Kids and Air Pollution
Kids and Air Pollution
 No Ordinary Joe
No Ordinary Joe Playing with Matches
Playing with Matches Skin In the Game
Skin In the Game



 Exercise in a Wrapper
Exercise in a Wrapper
 Down and Dirty
Down and Dirty Going Green
Going Green
 Is Paleo Diet Hard to Swallow?
Is Paleo Diet Hard to Swallow?
 Do you have a hot topic for Dr. D’Angelo and his Trinitas ER team?
Do you have a hot topic for Dr. D’Angelo and his Trinitas ER team? I’m In Agony…What Now?
I’m In Agony…What Now? There are, of course, conditions we see where we know right away that a cure is not possible. One such condition is when there is permanent nerve injury. In such cases, the goal is palliative care, to relieve as much of the pain and improve as much of the function as possible, using various interventional techniques and other modalities.
There are, of course, conditions we see where we know right away that a cure is not possible. One such condition is when there is permanent nerve injury. In such cases, the goal is palliative care, to relieve as much of the pain and improve as much of the function as possible, using various interventional techniques and other modalities. My MRI shows a disk herniation, do I need surgery?
My MRI shows a disk herniation, do I need surgery? Editor’s Note: Dr. Todd Koppel is a board-certified pain specialist and
Editor’s Note: Dr. Todd Koppel is a board-certified pain specialist and



 As Trinitas worked to stay a step ahead of the coronavirus this past spring and deliver a high level of healthcare to those who needed to be admitted, another part of the hospital—the Ambulatory Surgery Center (ASC)—was closed and waiting to safely reopen, and is now firing on all cylinders. “Ambulatory” in the case of the ASC reflects its Latin root (abulatore: to walk). The ASC is an outpatient facility that allows our clients to have same-day procedures. Although there is always some risk in any type of surgery, the layer-upon-layer of Covid-19 precautions that have been adopted, as Trinitas doctors learn more about the virus, has minimized the risk of contracting and spreading the virus in the main hospital as well.
As Trinitas worked to stay a step ahead of the coronavirus this past spring and deliver a high level of healthcare to those who needed to be admitted, another part of the hospital—the Ambulatory Surgery Center (ASC)—was closed and waiting to safely reopen, and is now firing on all cylinders. “Ambulatory” in the case of the ASC reflects its Latin root (abulatore: to walk). The ASC is an outpatient facility that allows our clients to have same-day procedures. Although there is always some risk in any type of surgery, the layer-upon-layer of Covid-19 precautions that have been adopted, as Trinitas doctors learn more about the virus, has minimized the risk of contracting and spreading the virus in the main hospital as well.
 The $5.2 million 9,500 square-foot Ambulatory Surgery Center opened in 2014. Since then, more than 10,000 patients have been treated there.
The $5.2 million 9,500 square-foot Ambulatory Surgery Center opened in 2014. Since then, more than 10,000 patients have been treated there.