How has the Human Genome Project changed the way we look at life?
By Christine Gibbs
The human body consists of more than 100 million million cells. Each contains a complete set of blueprints that determines who and what we are. Reading those blueprints was the goal of the Human Genome Project. By analyzing the sequence of the cellular gene pairs that make up that incredible macromolecule—our DNA—scientists hoped to unlock secrets that would lead to the prediction and prevention of future health issues, as well as designing treatments for all manner of diseases. The first significant results of the Human Genome Project were released to the public in 2003. Since then, an international army of biotech researchers has been using this information to explore the genetic differences that increase the risk for certain common diseases, such as diabetes and cancer, in order to develop effective cures and treatments.
When the Human Genome Project began, it laid out a set of ground rules for its participants:
- Identify all the genes in human DNA
- Sequence the chemical base pairs that make up human DNA
- Store this information in databases
- Improve the tools used to analyze this data
- Address the ethical, legal and social issues that are likely to arise and
- Transfer technologies to the private sector
Wait. What? That last item caught a lot of people off guard. Why would government-funded research centers in the US, UK, Japan, France, Germany and Spain simply hand over their breakthroughs to pharmaceutical companies and biotech firms? The directive to share technology with the private sector was originally intended to encourage friendly cooperation for the good of humankind. Needless to say, it actually generated some not-so-friendly competition—and, at times, near open warfare. Ironically, it was this rivalry that spurred some of the most productive research, and resulted in impressive scientific advances.
THE GREAT RACE
A case in point is J. Craig Venter, recognized as one of the most successful entrepreneurs in the genomics arena (he was included in 2008 on Time magazine’s list of the 100 most influential people in the world). Venter launched his career in bioscience with the Human Genome Project as a colleague of Dr. Francis Collins, who headed the National Human Genome Research Institute, which was formed under the National Institutes of Health. In his autobiography, A Life Decoded, Venter said he became frustrated with the slow pace of progress with the project, prompting him to fund his own company. To do so, he turned to Wallace Steinberg, a lifelong New Jersey resident and entrepreneurial visionary in the private sector. Steinberg was famously quoted in a 1992 New York Times article as saying, “I have this theory that death is a genetic disease.”

Photo credit: iStockphoto/Thinkstock
Together, Venter and Steinberg formed a non-profit research center, The Institute for Genomic Research (affectionately called TIGRE). The collaboration was nothing short of remarkable.
Venter’s corporate goal was to sequence the human genome and release it into the public domain faster and cheaper than the Human Genome Project itself. The pressure TIGRE put on the public program led to a redoubling of its efforts. In 2001, the Human Genome Project managed to publish its initial findings for the scientific community one day before Venter’s publication—three years before the project’s original target date. Yet the greater victory may belong to Venter. His “shotgun” approach to sequencing has become the de facto standard still used today. In truth, we are all the winners in this great race. Since then, the scientific advances from both the project and the private sector in deciphering the human genetic code have led to a wide range of improvements.
Topping the list of advances that have come from genetic research are those made in personalizing medical diagnosis, prognosis and treatment. Human genome mapping will soon become more available and popular as the cost (currently about $8,000) is reduced to a more affordable $1,000. That’s less than an MRI, which is mind-boggling when you consider that it cost the Human Genome Project about $400 million to sequence the first genome of a cancer cell. Already we are learning why certain cancer treatments are more effective than others—and that some patients may not be getting the best treatment at all.
Indeed, on a recent CBS This Morning segment, Dr. Sanjay Gupta reported that as much as one-third of current cancer patients are getting the “wrong” treatment for their particular type of cancer. Dr. Gupta explained that genomic mapping research should help reduce this percentage by pinpointing the best possible treatment regimens according to personal genetic markers.
A deeper understanding of the inner workings of DNA has led to breakthroughs that extend far beyond our own bodies. For instance, analyzing the genome structure of non-human species has resulted in raising hardier, healthier, and safer crops and animals. Through that pesky government requirement to share genome technology with the private sector there have been major improvements in the “greening” of many industries, resulting in cleaner and more efficient processing of chemicals, textiles, food products, fuels, and more. In the area of environmental biotechnology, genome technology has led to producing biodegradable products, finding new energy resources, and initiating hazardous site cleanup. And recently we learned that five major mental illnesses share a common genetic root—the result of the largest-ever genetic study of psychiatric disorders.
TOO MUCH INFORMATION
If you’re like most Americans, the greatest impact the Human Genome Project has had on your daily life is the TV crime show. You can’t turn the channel without finding an episode that hinges on the breathlessly awaited results
from the “DNA lab.” A whole new vocabulary has crept into our daily lives, as well as a whole new set of expectations. We are all experts, it would seem, in solving cases with technology developed during the Human Genome Project. In fact, cagey lawyers have made this awareness a part of criminal defense cases, elevating the burden of proof to the molecular level. “Where’s the DNA evidence?” they ask…and juries nod in agreement. Like most things on TV, it really doesn’t work that way. Most crime scenes produce no usable or relevant DNA.
That being said, criminology has benefited. Suspects in certain crimes can be ruled out, leaving police more time to focus on their investigations. And the guilty can be brought to justice where traditional evidence might prove inconclusive. Perhaps most important, the wrongfully imprisoned have been exonerated in significant numbers thanks to analysis of DNA evidence. In addition, anthropology has benefited. Paternity claims have been resolved through simple DNA smears. DNA can be used to match organ donors. And even national security has been impacted by improvements in detecting and resisting harmful biological warfare agents.
At what point, however, do we cross the line into the realm of too much information? How much about ourselves do we really want to know? The classic question is: “If your genome mapping raises the possibility of a serious disease lurking somewhere in your future—especially one for which there is currently no known treatment or cure, such as Alzheimer’s—would you want to know?” Regardless of the answer, the next question is: “Who else might find out?”
This raises the serious issue of privacy. The possible consequences are real. Insurance premiums might rise after the insurer is notified of a predisposition to a life-threatening illness. An employer might be less motivated to hire someone with a less than perfect genome profile. Colleges may reject students on the same basis. Once your genetic information has been published, the genie is out of the bottle, so to speak. The possibility exists that you could become a victim of genetic discrimination through unauthorized access to personal health records.
The primary weapon against such violations of privacy is HIPAA, the Health Insurance Portability and Accountability Act of 1996, which spells out your rights regarding personal health information, and limiting who may access and use that information. Yet medical identity theft can and does occur. According to a report released from the Ponemon Institute, a privacy and security research firm, it is a $30 billion a year crime in the United States.
While other American industries have been constricted by the recent recession, the genomics business has been fairly booming. Building off the Human Genome Project, researchers are breaking new ground every day. Even with recent budget cutbacks, as a nascent industry, genomics is building an impressive track record. Ernst & Young in 2011 reported that there were 1,870 public and private biotech companies in the U.S. alone, with annual revenues totaling $58.8 billion. A striking success story is Human Genome Sciences (HGS) which, with the backing of Goldman Sachs in 2009, raised more than $800 million through stock offerings. Competition is fierce. R&D is expensive. But potential profit can be irresistible.
Despite serious concerns such as medical identity theft and genetic engineering, the value added by the Human Genome Project to the quality of our lives is undeniable. Among its proponents is none other than Dr. Mehmet Oz, who encourages everyone to become familiar with their own genetic architecture. As he noted in a recent issue of O Magazine, “Our one-size-fits-all approach to medicine will soon be a thing of the past.” Of course, Dr. Oz tempers his enthusiasm with a not-unexpected caveat: Always work closely with your doctor.
 Genomics 101
Genomics 101
Let’s flex our left brain with some basic scientific vocabulary. Besides being a mouthful, the term Deoxyribonucleic Acid (or the more familiar short form DNA) is the chemical name for a macromolecule that encodes essential genetic instructions. These instructions determine the development of not only every single known organism, but many hazardous viruses, too.
Moving up the vocabulary ladder, a gene is the basic unit of inheritance passed on to us from each parent. Genes determine diverse personal traits, ranging from how we look to how we metabolize, how we fight infection and even how we behave. Individual genes (approximately 20,000 of them) reside on “packages” of DNA called chromosomes within a cell’s nucleus. Humans have 23 pairs of chromosomes, contributed by both parents, one of which determines sex—the X and Y chromosome.
The operative word in the Human Genome Project—a genome—is an aggregate of all of the aforementioned genetic information. The human genome is made up of the macromolecule DNA, which is the main component of our genes and chromosomes. The genome is simply “everything.”




 NO COMPARISON
NO COMPARISON
 Pretty exciting stuff back then—not to mention a field day for the special effects team.
Pretty exciting stuff back then—not to mention a field day for the special effects team.

 WATCH WHAT YOU EAT
WATCH WHAT YOU EAT
 Is Obesity the New Normal?
Is Obesity the New Normal? Deep 6 BPA
Deep 6 BPA Dr. Kevin Lukenda of Trinitas Regional Medical Center. “Responsible parents need to stay on top of—and be aware of—the possible downside of these conveniences. We need to always remind ourselves that certain products may make our lives easier…but need to know which of these advances can be a risk to our health.”
Dr. Kevin Lukenda of Trinitas Regional Medical Center. “Responsible parents need to stay on top of—and be aware of—the possible downside of these conveniences. We need to always remind ourselves that certain products may make our lives easier…but need to know which of these advances can be a risk to our health.” E-Lim-I-Nate the Negative
E-Lim-I-Nate the Negative Rodger Goddard, PhD, Chief Psychologist and Director of Wellness Management Services at Trinitas. Dr. Goddard adds that controlling stress should be very high on one’s priority list. “We cannot become monks and live in a cave in the mountains, so we need to deal productively with what is in our lives,” he says. Stress management involves using both passive and active tools and skills. Passive skills involve improving the capacity to calm our body and muscles down all throughout the day, and involve deep-breathing, stretching, muscle softening and self-calming thoughts all day long. Active skills involves using:
Rodger Goddard, PhD, Chief Psychologist and Director of Wellness Management Services at Trinitas. Dr. Goddard adds that controlling stress should be very high on one’s priority list. “We cannot become monks and live in a cave in the mountains, so we need to deal productively with what is in our lives,” he says. Stress management involves using both passive and active tools and skills. Passive skills involve improving the capacity to calm our body and muscles down all throughout the day, and involve deep-breathing, stretching, muscle softening and self-calming thoughts all day long. Active skills involves using: Your Germs, My Germs
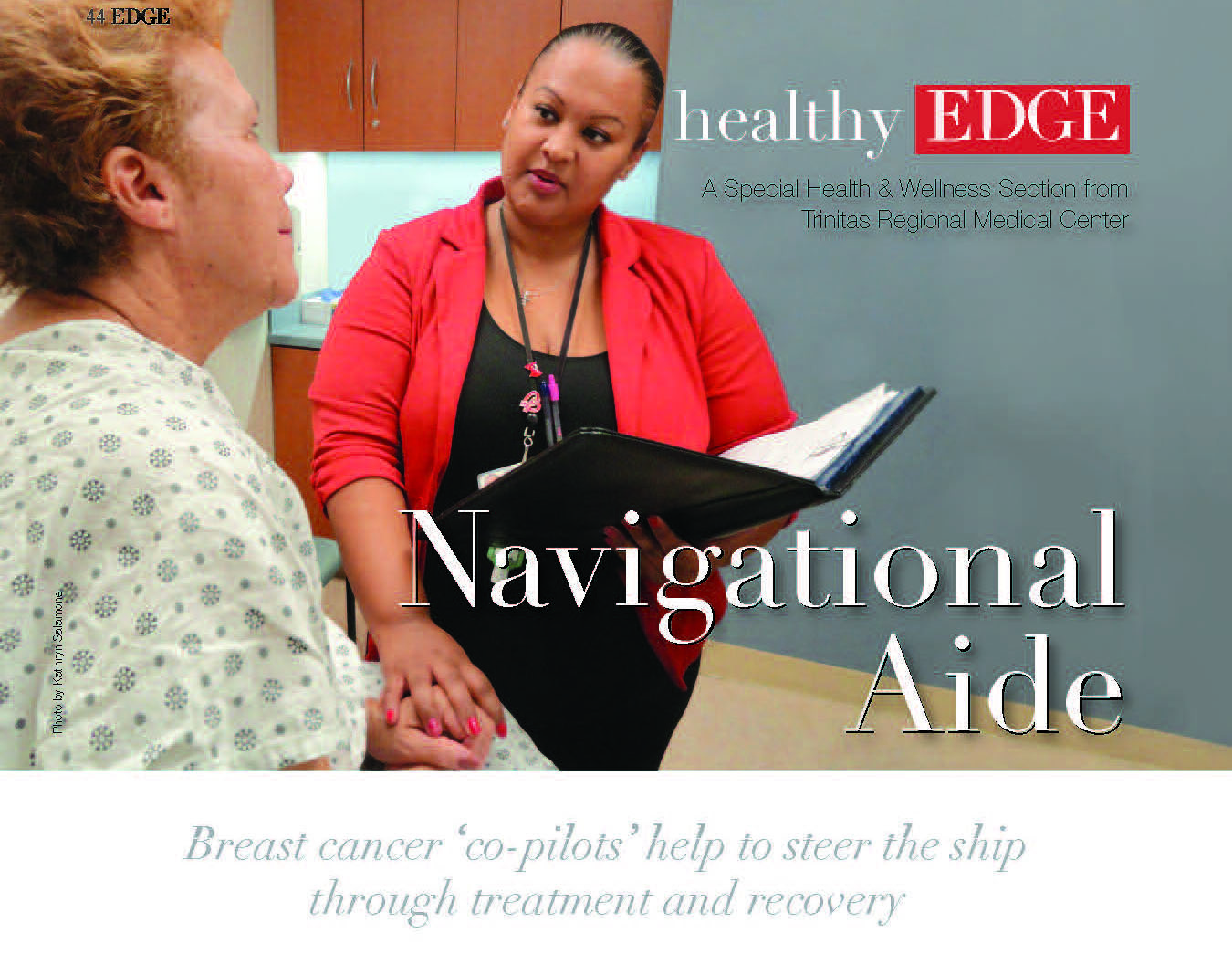
Your Germs, My Germs Michelle Gillis-Harry, RN, MPH, CIC, Director of Infection Prevention and Control at Trinitas. “By using a sanitizing spray or a disinfectant wipe that kills germs, you create a line of defense against germs that others leave behind. But, based on the findings of this study, as you close the hotel door behind you, you’re leaving your own unique microbial imprint. Simply put, we all leave our mark on the places we live, visit, work or play. It’s part of being human and living within the complex environment we call the Earth.” The true potential of the Chicago study (and others in the works) may be in forensics, since microbiological evidence left by humans may be more useful than fingerprints.
Michelle Gillis-Harry, RN, MPH, CIC, Director of Infection Prevention and Control at Trinitas. “By using a sanitizing spray or a disinfectant wipe that kills germs, you create a line of defense against germs that others leave behind. But, based on the findings of this study, as you close the hotel door behind you, you’re leaving your own unique microbial imprint. Simply put, we all leave our mark on the places we live, visit, work or play. It’s part of being human and living within the complex environment we call the Earth.” The true potential of the Chicago study (and others in the works) may be in forensics, since microbiological evidence left by humans may be more useful than fingerprints. Trinitas Joins Elite Group of Palliative Care Programs
Trinitas Joins Elite Group of Palliative Care Programs



 Root Causes
Root Causes


 Bariatric Surgery: A “Miracle Moment”
Bariatric Surgery: A “Miracle Moment” Heads Up On Facial Fractures
Heads Up On Facial Fractures Crazy Time for Cannabis
Crazy Time for Cannabis Link Between Sleep Disorders and Cancer Deaths
Link Between Sleep Disorders and Cancer Deaths Environmental Factors Trigger Allergies in Newborns
Environmental Factors Trigger Allergies in Newborns Holiday Baking: Shoulda Woulda Coulda
Holiday Baking: Shoulda Woulda Coulda New Findings on Gluten-Free Foods
New Findings on Gluten-Free Foods Raisin D’Etre
Raisin D’Etre


 Good News for Popeye
Good News for Popeye
 I Can’t Believe It’s Not Healthy
I Can’t Believe It’s Not Healthy
 Nickel for Your Thoughts
Nickel for Your Thoughts Mouth to Mouth
Mouth to Mouth
 Now You See Me
Now You See Me Weighty Issues
Weighty Issues
 Red Hot News on Chili Peppers
Red Hot News on Chili Peppers
 The six ways to assess a problem are by looking at the areas of Thought, Emotion, Action, Frequency, Duration and Intensity. Thought refers to how we think about and view our problem. Are our thoughts, for example, helping to solve our problem? Or are they self-critical, condemning or working against us and therefore exaggerating or making our problem worse? Emotion refers to the feelings that a problem brings up in us, and how we handle those feelings. Can we name what we are feeling (e.g. sad, anxious, guilty, angry, insecure, shame or rage)? Are we able to make friends with our feelings and get information from them about what we want and need? Or do we let our emotions overwhelm and injure our health? Action refers to the positive or negative behaviors that we do in response to our problem. Does our problem lead us to say bad things to people—or try to shop, drink, smoke, drug or eat our problem away? Frequency refers to how often a problem or difficulty occurs. Does it trouble us once a month, week, day, hour or minute? Duration refers to how long our problem lasts when it comes. Does it cause us to feel bad for a couple of minutes and then go away, or do we feel terrible for hours, days, weeks, months or years? Finally, Intensity refers to the degree of distress the problem causes. Does it lead us to be mildly uncomfortable and irritable, or so intensely upset that we are ready to explode?
The six ways to assess a problem are by looking at the areas of Thought, Emotion, Action, Frequency, Duration and Intensity. Thought refers to how we think about and view our problem. Are our thoughts, for example, helping to solve our problem? Or are they self-critical, condemning or working against us and therefore exaggerating or making our problem worse? Emotion refers to the feelings that a problem brings up in us, and how we handle those feelings. Can we name what we are feeling (e.g. sad, anxious, guilty, angry, insecure, shame or rage)? Are we able to make friends with our feelings and get information from them about what we want and need? Or do we let our emotions overwhelm and injure our health? Action refers to the positive or negative behaviors that we do in response to our problem. Does our problem lead us to say bad things to people—or try to shop, drink, smoke, drug or eat our problem away? Frequency refers to how often a problem or difficulty occurs. Does it trouble us once a month, week, day, hour or minute? Duration refers to how long our problem lasts when it comes. Does it cause us to feel bad for a couple of minutes and then go away, or do we feel terrible for hours, days, weeks, months or years? Finally, Intensity refers to the degree of distress the problem causes. Does it lead us to be mildly uncomfortable and irritable, or so intensely upset that we are ready to explode? Saturn is the God of time. People who use a Saturn strategy—Strategy #6—take time to digest and respond to their problems. This involves patience, long-term planning and Steady, Patient Work over a long period of time. They know that continual small actions enable them to change a situation, whether it’s something about themselves, another person or a relationship.
Saturn is the God of time. People who use a Saturn strategy—Strategy #6—take time to digest and respond to their problems. This involves patience, long-term planning and Steady, Patient Work over a long period of time. They know that continual small actions enable them to change a situation, whether it’s something about themselves, another person or a relationship. Editor’s Note: Dr. Rodger Goddard has served as the Chief Psychologist at Trinitas Regional Medical Center for over 25 years. He is the director of Wellness Management Services, which provides workshops, presentations and programs to companies and schools to improve individual and organizational success. He is also the director of the hospital’s APA-accredited psychology internship program. He can be reached at rgoddard@trinitas.org or (908) 994-7334.
Editor’s Note: Dr. Rodger Goddard has served as the Chief Psychologist at Trinitas Regional Medical Center for over 25 years. He is the director of Wellness Management Services, which provides workshops, presentations and programs to companies and schools to improve individual and organizational success. He is also the director of the hospital’s APA-accredited psychology internship program. He can be reached at rgoddard@trinitas.org or (908) 994-7334.

 Trinitas has successfully integrated advanced emergency lifesaving treatment methods into the emergency angioplasty treatment process, Dr. D’Angelo points out. “Our team effort uses a ’30-30-30’ rhythm. 30 minutes for EMS responders to reach the patient, perform an EKG, and get the patient to us. 30 minutes for the Emergency Team to receive, stabilize and transport the patient to the cath lab. Then, 30 minutes for the Catheterization Team to open the occluded artery.”
Trinitas has successfully integrated advanced emergency lifesaving treatment methods into the emergency angioplasty treatment process, Dr. D’Angelo points out. “Our team effort uses a ’30-30-30’ rhythm. 30 minutes for EMS responders to reach the patient, perform an EKG, and get the patient to us. 30 minutes for the Emergency Team to receive, stabilize and transport the patient to the cath lab. Then, 30 minutes for the Catheterization Team to open the occluded artery.”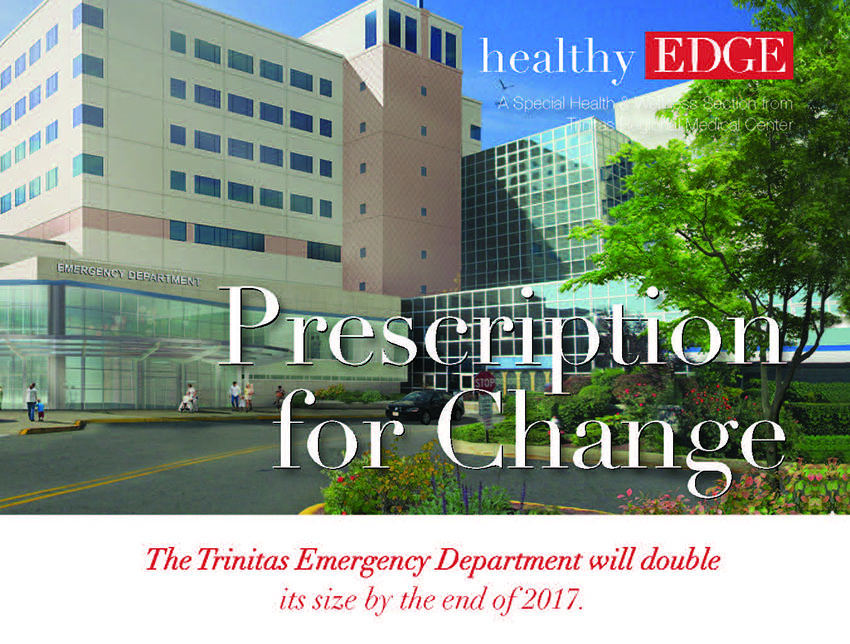


 Andrea S. Zimmern, MD, FACS
Andrea S. Zimmern, MD, FACS
 Do you have a hot topic for Dr. D’Angelo and his Trinitas ER team?
Do you have a hot topic for Dr. D’Angelo and his Trinitas ER team?
 Experimental Drug Looks Good vs. MRSA
Experimental Drug Looks Good vs. MRSA
 A Blunt Assessment of Marijuana
A Blunt Assessment of Marijuana
 Obesity and the Brain
Obesity and the Brain
 Part of the shifting treatment landscape for Behavioral Health stems from what Dr. Salvatore Savatta, Chair of Psychiatry at Trinitas, calls a “dramatic expansion” over the last 15 years in relevant research and the volume of information sources from which practitioners can draw:
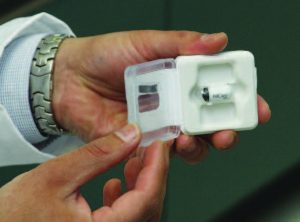
Part of the shifting treatment landscape for Behavioral Health stems from what Dr. Salvatore Savatta, Chair of Psychiatry at Trinitas, calls a “dramatic expansion” over the last 15 years in relevant research and the volume of information sources from which practitioners can draw: Esketamine is a more potent and faster-acting form of ketamine, which is most often used as a surgical anesthetic and has been around for 50 years. Esketamine has an immediate effect on treatment-resistant depression and also appears to reduce suicide ideation. Delivering the drug in a nasal spray means it is absorbed by a different receptor than pills are—providing a much faster route to the brain, where it targets multiple brain connections at once.
Esketamine is a more potent and faster-acting form of ketamine, which is most often used as a surgical anesthetic and has been around for 50 years. Esketamine has an immediate effect on treatment-resistant depression and also appears to reduce suicide ideation. Delivering the drug in a nasal spray means it is absorbed by a different receptor than pills are—providing a much faster route to the brain, where it targets multiple brain connections at once.
 During her high school years at Union County Vo-Tech’s Allied Health School, Jones took part in a Medical Mentoring program and Nursing Camp at Trinitas, laying the foundation of skills and academics on which she built her professional plans. Her undergraduate studies at Drexel University—funded partly by a scholarship from Trinitas—propelled her ever forward and enhanced her passion for the business of healthcare.
During her high school years at Union County Vo-Tech’s Allied Health School, Jones took part in a Medical Mentoring program and Nursing Camp at Trinitas, laying the foundation of skills and academics on which she built her professional plans. Her undergraduate studies at Drexel University—funded partly by a scholarship from Trinitas—propelled her ever forward and enhanced her passion for the business of healthcare. 
 That experience planted another seed for Jasmine Jones: the possibility of one day putting her journalism skills to use by traveling the world, tracking her experiences in a memoir, and using her expertise to impact healthcare policy. At the moment, as one of Trinitas’s promising new Emergency Department RNs, she’ll remain close to home and family. Her own, as well as the Trinitas family…which she’s been a part of now going on ten years.
That experience planted another seed for Jasmine Jones: the possibility of one day putting her journalism skills to use by traveling the world, tracking her experiences in a memoir, and using her expertise to impact healthcare policy. At the moment, as one of Trinitas’s promising new Emergency Department RNs, she’ll remain close to home and family. Her own, as well as the Trinitas family…which she’s been a part of now going on ten years. 