10 Ways to Live Longer (and Better)
You may be one of the 47% who “doesn’t pay taxes,” but that other inevitability—death—is a little harder to sidestep. Indeed, sooner or later the predator time catches us all. The trick, of course, is to push “later” as far forward as possible. We do this by eating well, exercising and not smoking. At least, that is what we are told to do. The reality is quite different. According to the CDC, one third of our population qualifies as obese, and a Duke University study projects a rise to 42% by 2030—adding $550 billion to national healthcare obligations. With obesity running rampant through America, some of us actually breathe a sigh of relief that we are merely “overweight.” Meanwhile, we spend billions on exercise equipment that gathers more dust than sweat, gym memberships that can’t be cancelled, and workout wardrobes that still have their tags on—more than $70 billion a year, according to the Sporting Goods Manufacturers Association. And although we have come a long way from idolizing the Marlboro Man and athletes sponsored by Virginia Slims, smoking is actually on the rise among women and teens. We all know what to do. So why aren’t we doing it? What is it that triggers yo-yo dieting, couch potato-ing, and closet smoking? We all want to live longer…so why are we so bad at it? In many cases, it turns out, the prospect of making major life changes is so daunting or dispiriting that folks unconsciously have given up before they even begin; one bump in the road and they revert back to bad habits. A successful outcome is far more likely if you take on small, achievable challenges and fold them into your current lifestyle. In that spirit, we’ve identified 10 smart ways to keep you going strong:
1 DRINK UP The Mayo Clinic has adjusted the longstanding “8 by 8” rule (eight 8-ounce glasses of water daily) to include any healthy fluids. And a Loma Linda University study indicates that as little as 5-8 ounces daily can be helpful.
2 SWEET SURRENDER According to a 15-year study conducted by Dutch researchers, eating about 4 grams of cocoa a day could cut your risk of heart disease. Dark chocolate with a high cocoa content is ideal.
3 LAUGHTER IS THE BEST MEDICINE According to a study by Dr. Michael Miller at the University of Maryland, laughter can reduce blood pressure, lower cholesterol and improve blood flow to the heart by as much as 50%. Start DVR-ing The Colbert Report!
4 ACID TEST The International Journal of Cardiology tells us that chronic heartburn can lead to a heart attack. A high acid level in the esophagus, when untreated, can decrease blood flow to the heart by 20%. According to a CNN report last year, if you suffer from heartburn you might try sleeping on your side to reduce acid reflux.
5 CATCH SOME Zs According to the CDC, 41 million Americans don’t get enough sleep, with consequences ranging from a higher risk of diabetes to depression to slower reaction time in emergencies. How much sleep is right for you? The next time you have a totally free weekend—or better yet, a vacation—go to bed when you’re tired and wake up when you want. If you get through the day without feeling tired, that’s probably your “sleep number.”
6 CURRY FLAVOR Rutgers University scientists have determined that combining curry with cruciferous vegetables (cabbage, bok choi, turnips, broccoli, cauliflower) appears to help ward off prostate cancer.
7 GO NUTS Loma Linda University researchers tracking the lifestyle habits of 34,000 Seventh-Day Adventists (a population famous for its longevity), discovered that those who munched on two ounces of nuts almost daily lived on average almost three years longer.
8 PERK UP Numerous studies have linked coffee drinking (often 2-3 cups per day) with a positive impact on diabetes, heart attacks and strokes—and even Parkinson’s and Alzheimer’s.
9 STAND UP FOR YOURSELF Whether in front of the TV, computer or anywhere, sitting for long periods at work or at home can be almost as risky as smoking or being obese, particularly for your heart. Dr. James Levine, a professor at the Mayo Clinic, suggests that even sitting for an hour straight is sitting too long.
10 THINK POSITIVE A Yale University study of older adults showed that those with a positive outlook on aging lived about seven years longer than those with less optimism.
Dr. Kevin Lukenda, who chairs the Family Medicine Department at Trinitas, also believes in keeping things simple. He advises his patients to live by the following 10 rules:
1 Reduce stress by not taking anything too seriously.
2 Set aside quality time with friends and family; share your feelings, thoughts and fears with them.
3 Do something selfish and productive for 15 minutes every day.
3a Do something selfish and productive for one hour once a week.
4 Read a book, magazine, newspaper—anything.
5 Do nothing to the extreme.
6 Keep your carbs to a minimum.
7 Get enough sleep!
8 Life is hard—be a strong person rather than asking for an easier life.
9 Take walks.
10 See your family doctor as needed. Regardless of which (or whose) nuggets of wisdom you follow, the good news is that you have a lot of interesting and attainable options. Still better news is that some of them you might even enjoy! The best news? All of these not only add up to living longer. They add up to living better.
Editor’s Note: Log onto edgemagonline.com for six more ambitious ways to improve and extend your life.


 Don’t Just Sit There! Thanks to a new study out of Australia, you can add one more thing to the list of long-term health no-no’s that includes smoking, drinking, lack of exercise and a high-fat diet: Sitting. Research by the Sax Institute of adults 45 and over found that those who sat for 11 or more hours a day had a 40% higher risk of dying within the next three years than people who sat less than four hours a day. The study adjusted for an array of other lifestyle and medical issues, but even for those who exercised regularly, the risk of death still rose with every additional hour spent in a chair.
Don’t Just Sit There! Thanks to a new study out of Australia, you can add one more thing to the list of long-term health no-no’s that includes smoking, drinking, lack of exercise and a high-fat diet: Sitting. Research by the Sax Institute of adults 45 and over found that those who sat for 11 or more hours a day had a 40% higher risk of dying within the next three years than people who sat less than four hours a day. The study adjusted for an array of other lifestyle and medical issues, but even for those who exercised regularly, the risk of death still rose with every additional hour spent in a chair. New Road Map for Families of Teen Diabetics For many parents, coping day-to-day with their teenagers is the most difficult, aggravating and exhausting phase of the child-rearing process. For parents of teens with Type 1 Diabetes, managing the disease and the young man or woman can prove next to impossible. The Eunice Kennedy Shriver National Institute of Child Health and Human Development recently provided a road map that families should find helpful. Their findings suggest that kids between ages 12 and 15 with Type 1 Diabetes benefitted dramatically from a two-year program (of three to four meetings a year) with parents and a health advisor to discuss shared responsibilities, goals and strategies for solving diabetes management problems that arose. Meeting with a health advisor during regular diabetes clinic visits, researchers reported, helped families better manage the changes that occur as children take on more responsibility for their day-to-day diabetes care.
New Road Map for Families of Teen Diabetics For many parents, coping day-to-day with their teenagers is the most difficult, aggravating and exhausting phase of the child-rearing process. For parents of teens with Type 1 Diabetes, managing the disease and the young man or woman can prove next to impossible. The Eunice Kennedy Shriver National Institute of Child Health and Human Development recently provided a road map that families should find helpful. Their findings suggest that kids between ages 12 and 15 with Type 1 Diabetes benefitted dramatically from a two-year program (of three to four meetings a year) with parents and a health advisor to discuss shared responsibilities, goals and strategies for solving diabetes management problems that arose. Meeting with a health advisor during regular diabetes clinic visits, researchers reported, helped families better manage the changes that occur as children take on more responsibility for their day-to-day diabetes care. Impact of the NYC Soda Ban The announcement of an impending ban in New York City on large, sugary drinks has prompted many people—both inside and outside of the medical profession—to chime in on what, if any, effects this will have on overall health. Obviously, gulping down quarts of soda, energy drinks and sweetened teas a week is not a smart idea. But will shaving a few ounces off this total make a difference? The consensus thus far is that it will—but only a small difference. Obesity is a complex disease, involving a lot of variables. That being said, if the “soda ban” pushes forward the national discussion about the dangers of consuming too much sugar—and overeating in general—it could have a significant impact. Lifestyle changes are often triggered by cultural changes; if the culture of junk-food consumption is altered through publicity and awareness that begins in New York, we may look back on this law as a true game-changer.
Impact of the NYC Soda Ban The announcement of an impending ban in New York City on large, sugary drinks has prompted many people—both inside and outside of the medical profession—to chime in on what, if any, effects this will have on overall health. Obviously, gulping down quarts of soda, energy drinks and sweetened teas a week is not a smart idea. But will shaving a few ounces off this total make a difference? The consensus thus far is that it will—but only a small difference. Obesity is a complex disease, involving a lot of variables. That being said, if the “soda ban” pushes forward the national discussion about the dangers of consuming too much sugar—and overeating in general—it could have a significant impact. Lifestyle changes are often triggered by cultural changes; if the culture of junk-food consumption is altered through publicity and awareness that begins in New York, we may look back on this law as a true game-changer. Genetic Connection to Blindness More than 15 million people around the world suffer from blindness brought on by Primary Angle Closure Glaucoma (PACG). The problem is especially pronounced among Asian populations, which account for about 12 million of these cases. A collaborative international research effort launched in Singapore recently identified three previously unknown genes associated with PACG. The medical community has long suspected the disease to be strongly hereditary, but these findings—published in the journal Nature Genetics—confirm the fact. This opens the door to possibilities of novel treatments, as well as the potential of early identification of people at risk for PACG. “These data are the first critical steps toward a better understanding of the underlying molecular events responsible for this blinding disease,” explains Dr. Janey Wiggs, Professor of Ophthalmology at Harvard Medical School.
Genetic Connection to Blindness More than 15 million people around the world suffer from blindness brought on by Primary Angle Closure Glaucoma (PACG). The problem is especially pronounced among Asian populations, which account for about 12 million of these cases. A collaborative international research effort launched in Singapore recently identified three previously unknown genes associated with PACG. The medical community has long suspected the disease to be strongly hereditary, but these findings—published in the journal Nature Genetics—confirm the fact. This opens the door to possibilities of novel treatments, as well as the potential of early identification of people at risk for PACG. “These data are the first critical steps toward a better understanding of the underlying molecular events responsible for this blinding disease,” explains Dr. Janey Wiggs, Professor of Ophthalmology at Harvard Medical School. New Study on Job Stress When Johnny Paycheck recorded the country hit “Take This Job and Shove It” back in the 1970s, it turns out he was way ahead of his time. Doctors in England recently completed a study that shows workers who feel over-pressured yet powerless run a risk of coronary disease that is 23% greater than those who are content in their work environment. The study covered around 200,000 workers in a wide range of occupations, from civil servants to factory workers. Subjects were asked about the type of work they did, the workload, deadlines and freedom to make decisions.
New Study on Job Stress When Johnny Paycheck recorded the country hit “Take This Job and Shove It” back in the 1970s, it turns out he was way ahead of his time. Doctors in England recently completed a study that shows workers who feel over-pressured yet powerless run a risk of coronary disease that is 23% greater than those who are content in their work environment. The study covered around 200,000 workers in a wide range of occupations, from civil servants to factory workers. Subjects were asked about the type of work they did, the workload, deadlines and freedom to make decisions.





 Editor’s Note: Jim Dunleavy is the Director of Physical Therapy and Rehabilitation for Trinitas Regional Medical Center.
Editor’s Note: Jim Dunleavy is the Director of Physical Therapy and Rehabilitation for Trinitas Regional Medical Center.
 The Ankle Bone’s Connected to the…What? That broken ankle may lead to bigger problems. So say researchers at Texas Tech, who recently established a link between ankle injuries and life-threatening complications, including deep vein thrombosis and pulmonary embolisms. The study suggested that treating physicians should assess patients with ankle fracture for their risk of developing a venous thromboembolic event on an individual basis, and also provide thromboprophylaxis (prevention of thrombosis) for those with an increased risk of developing such complications.
The Ankle Bone’s Connected to the…What? That broken ankle may lead to bigger problems. So say researchers at Texas Tech, who recently established a link between ankle injuries and life-threatening complications, including deep vein thrombosis and pulmonary embolisms. The study suggested that treating physicians should assess patients with ankle fracture for their risk of developing a venous thromboembolic event on an individual basis, and also provide thromboprophylaxis (prevention of thrombosis) for those with an increased risk of developing such complications. Let’s Do (it at) Lunch As a rule, people don’t mind paying the tab to achieve healthy, beautiful skin. Finding the time to make it happen is often the greater obstacle. According to plastic surgeon Dr. Joseph D. Alkon, there are a number of non-invasive, “lunchtime” treatments that can make your skin look and feel its best. “A chemical peel helps those with dry skin, uneven tone, acne, discoloration and/or mild wrinkles,” Dr. Alkon says. “This office-based procedure uses a special liquid to remove the harsh outer layers of skin, while leaving smoother and healthier layers intact. Peels vary from mild to aggressive depending on the skin being treated.” Microdermabrasion also works to remove unhealthy, dry, flaky outer skin, he adds. This procedure uses a gentle tool or wand to remove the outer layers of skin. This leaves behind fresh, healthy skin. Although commonly performed on the face, other body parts can benefit from both chemical peels and microdermabrasion. “A facial is another popular, relaxing and rejuvenating service,” Dr. Alkon says. “It’s often performed by a licensed esthetician, and includes a skin analysis followed by customized exfoliation, extraction, massage, and application of toners, moisturizers, and sunscreens customized to your skin type. A facial can leave the skin clean, clear, hydrated, and rejuvenated.”
Let’s Do (it at) Lunch As a rule, people don’t mind paying the tab to achieve healthy, beautiful skin. Finding the time to make it happen is often the greater obstacle. According to plastic surgeon Dr. Joseph D. Alkon, there are a number of non-invasive, “lunchtime” treatments that can make your skin look and feel its best. “A chemical peel helps those with dry skin, uneven tone, acne, discoloration and/or mild wrinkles,” Dr. Alkon says. “This office-based procedure uses a special liquid to remove the harsh outer layers of skin, while leaving smoother and healthier layers intact. Peels vary from mild to aggressive depending on the skin being treated.” Microdermabrasion also works to remove unhealthy, dry, flaky outer skin, he adds. This procedure uses a gentle tool or wand to remove the outer layers of skin. This leaves behind fresh, healthy skin. Although commonly performed on the face, other body parts can benefit from both chemical peels and microdermabrasion. “A facial is another popular, relaxing and rejuvenating service,” Dr. Alkon says. “It’s often performed by a licensed esthetician, and includes a skin analysis followed by customized exfoliation, extraction, massage, and application of toners, moisturizers, and sunscreens customized to your skin type. A facial can leave the skin clean, clear, hydrated, and rejuvenated.”  New Alzheimer’s Drug May Be on Horizon The medical profession has accepted the fact that there is no “cure” for Alzheimer’s. However, a trial just concluded found that patients who had injections every two weeks of the drug immunoglobulin—made from antibodies in human blood—showed no decline in cognition, memory, daily functioning or mood for a period of three years. Immunoglobulin is normally given to patients who suffer from an immune deficiency, and is extremely costly. If all goes well, however, the drug would be on the market within 10 years. “This is probably the most exciting drug we know about that is currently in the late stages of research,” says Clive Ballard, Director of Research at the Alzheimer’s Society. “We now know it is safe. But the real test will be whether these initial promising results can subsequently be replicated in larger groups.” As life spans increase, the likelihood that a person over the age of 65 will develop some form of dementia is about one in three. Currently, there are only three drugs for Alzheimer’s in the early to moderate stages, and they are effective in some patients but not in others.
New Alzheimer’s Drug May Be on Horizon The medical profession has accepted the fact that there is no “cure” for Alzheimer’s. However, a trial just concluded found that patients who had injections every two weeks of the drug immunoglobulin—made from antibodies in human blood—showed no decline in cognition, memory, daily functioning or mood for a period of three years. Immunoglobulin is normally given to patients who suffer from an immune deficiency, and is extremely costly. If all goes well, however, the drug would be on the market within 10 years. “This is probably the most exciting drug we know about that is currently in the late stages of research,” says Clive Ballard, Director of Research at the Alzheimer’s Society. “We now know it is safe. But the real test will be whether these initial promising results can subsequently be replicated in larger groups.” As life spans increase, the likelihood that a person over the age of 65 will develop some form of dementia is about one in three. Currently, there are only three drugs for Alzheimer’s in the early to moderate stages, and they are effective in some patients but not in others. Smile and Say “Aaaaaah” Do you experience nausea, bloating, heartburn, constipation, or a feeling of fullness? These may be symptoms of a motility disorder, such as gastroparesis and chronic constipation. Gastropathy is a common condition in long standing diabetic people, especially if not well controlled. People with gastropathy can suffer from postprandial indigestion, abdominal discomfort, nausea, and vomiting. Fortunately, the guesswork has been removed from diagnosis of these conditions thanks to the SmartPill, a wireless motility capsule procedure. “The SmartPill capsule travels through your GI tract, collects data, which is then recorded for your doctor to evaluate,” explains Samiappan Muthusamy M.D. of the Center for Digestive Diseases (cddnj.com), which offers this state-of-the art procedure. According to Dr. Muthusamy, the SmartPill can also diagnose Diffuse Colonic Dysfunction (aka lack of colon motility), an extremely serious condition that can present as constipation. Of course, causes such as a poor diet, lack of fluids, sluggish thyroid, colon cancer and constipating medications are ruled out first. “In modern medicine,” adds Dr. Muthusamy, “living with gastropathy and constipation is a thing of the past. They are treatable.”
Smile and Say “Aaaaaah” Do you experience nausea, bloating, heartburn, constipation, or a feeling of fullness? These may be symptoms of a motility disorder, such as gastroparesis and chronic constipation. Gastropathy is a common condition in long standing diabetic people, especially if not well controlled. People with gastropathy can suffer from postprandial indigestion, abdominal discomfort, nausea, and vomiting. Fortunately, the guesswork has been removed from diagnosis of these conditions thanks to the SmartPill, a wireless motility capsule procedure. “The SmartPill capsule travels through your GI tract, collects data, which is then recorded for your doctor to evaluate,” explains Samiappan Muthusamy M.D. of the Center for Digestive Diseases (cddnj.com), which offers this state-of-the art procedure. According to Dr. Muthusamy, the SmartPill can also diagnose Diffuse Colonic Dysfunction (aka lack of colon motility), an extremely serious condition that can present as constipation. Of course, causes such as a poor diet, lack of fluids, sluggish thyroid, colon cancer and constipating medications are ruled out first. “In modern medicine,” adds Dr. Muthusamy, “living with gastropathy and constipation is a thing of the past. They are treatable.” UGNJ Strikes Gold The Urology Group of New Jersey (UGNJ) recently earned The Joint Commission’s Gold Seal of Approval for its continuous standards of healthcare quality and safety in ambulatory care. By receiving this accreditation award, UGNJ is now the only Urology physician practice in the nation to achieve this status. Recognition followed a rigorous unannounced on-site survey of all 12 UGNJ offices in March 2012 by a team of expert surveyors, who evaluated the group’s standards of care specific to the needs of patients—including prevention of infection, leadership and medication management. “Achieving accreditation from The Joint Commission is a team effort that will bring confidence to our patients and give us a framework to provide the best care possible,” says Dr. Alan Krieger, UGNJ’s President.
UGNJ Strikes Gold The Urology Group of New Jersey (UGNJ) recently earned The Joint Commission’s Gold Seal of Approval for its continuous standards of healthcare quality and safety in ambulatory care. By receiving this accreditation award, UGNJ is now the only Urology physician practice in the nation to achieve this status. Recognition followed a rigorous unannounced on-site survey of all 12 UGNJ offices in March 2012 by a team of expert surveyors, who evaluated the group’s standards of care specific to the needs of patients—including prevention of infection, leadership and medication management. “Achieving accreditation from The Joint Commission is a team effort that will bring confidence to our patients and give us a framework to provide the best care possible,” says Dr. Alan Krieger, UGNJ’s President. Mapping Menopause A study published in July by the Endocrine Society suggests that the primary barrier to women receiving hormone therapy to treat menopausal symptoms is patients’ fears about the risks, and their unwillingness to discuss the option. What is interesting about this study is that it was conducted with internal medicine, family practice and OB/GYN physicians—and not patients. “Nearly every physician participating in the survey said menopausal symptoms have a negative impact on quality of life,” says William F. Young, Jr., MD, president of The Endocrine Society. “It’s important for a woman to know what hormonal and non-hormonal treatment options may be best for them to provide symptom relief.” To that end, the Society has created what it calls the Menopause Map, an online interactive tool that guides a woman through the different options available to get relief from her symptoms. The map uses a series of prompting questions about those symptoms and her personal health history, and also has links to questionnaires that help assess current risk for breast cancer, heart disease, and stroke. The tool weighs hormonal and non-hormonal therapies against the risks based on individual symptoms and medical history. The url is hormone.org/MenopauseMap.
Mapping Menopause A study published in July by the Endocrine Society suggests that the primary barrier to women receiving hormone therapy to treat menopausal symptoms is patients’ fears about the risks, and their unwillingness to discuss the option. What is interesting about this study is that it was conducted with internal medicine, family practice and OB/GYN physicians—and not patients. “Nearly every physician participating in the survey said menopausal symptoms have a negative impact on quality of life,” says William F. Young, Jr., MD, president of The Endocrine Society. “It’s important for a woman to know what hormonal and non-hormonal treatment options may be best for them to provide symptom relief.” To that end, the Society has created what it calls the Menopause Map, an online interactive tool that guides a woman through the different options available to get relief from her symptoms. The map uses a series of prompting questions about those symptoms and her personal health history, and also has links to questionnaires that help assess current risk for breast cancer, heart disease, and stroke. The tool weighs hormonal and non-hormonal therapies against the risks based on individual symptoms and medical history. The url is hormone.org/MenopauseMap.
 beach the following summer resulted in the wound festering still further into a situation so serious that it could easily have become limb-threatening. Out of sheer frustration and in near panic, Schroeding resorted to doing his own research on the Internet and identified two out-of-state hospitals with highly renowned wound care centers: Johns Hopkins in Baltimore and Trinitas Regional Medical Center in Elizabeth. The Hopkins website cited a 60-70% heal rate, whereas Trinitas claimed more than 90% overall. That made the choice easy.
beach the following summer resulted in the wound festering still further into a situation so serious that it could easily have become limb-threatening. Out of sheer frustration and in near panic, Schroeding resorted to doing his own research on the Internet and identified two out-of-state hospitals with highly renowned wound care centers: Johns Hopkins in Baltimore and Trinitas Regional Medical Center in Elizabeth. The Hopkins website cited a 60-70% heal rate, whereas Trinitas claimed more than 90% overall. That made the choice easy.
 Don’t Walk Sign Are you a sleepwalker? If so, you’re definitely not alone. New research by the Stanford University School of Medicine found that somnambulism is far more prevalent than previous studies suggested. About 3.6 percent of American adults are prone to nocturnal wandering. That translates to 8.4 million. The same research suggests that sleepwalking is linked to anxiety and depression. A subject of humor and silliness in popular culture, this disorder can actually have serious consequences. Sleepwalkers have been known to injure themselves and others. They are also prone to psychosocial disorders. The Trinitas Sleep Disorders Center deals with sleepwalking and other problems every day. For information call 908-994-8694.
Don’t Walk Sign Are you a sleepwalker? If so, you’re definitely not alone. New research by the Stanford University School of Medicine found that somnambulism is far more prevalent than previous studies suggested. About 3.6 percent of American adults are prone to nocturnal wandering. That translates to 8.4 million. The same research suggests that sleepwalking is linked to anxiety and depression. A subject of humor and silliness in popular culture, this disorder can actually have serious consequences. Sleepwalkers have been known to injure themselves and others. They are also prone to psychosocial disorders. The Trinitas Sleep Disorders Center deals with sleepwalking and other problems every day. For information call 908-994-8694.

 Another Link Between TV & Obesity From the “Wait, Didn’t We Know that Already?” department comes the news that kids who watch a lot of TV have poorer overall diets than kids whose exposure to television is limited. “The more TV you watch, the less likely you were to eat fruits and vegetables every day, and the more likely you were to eat things like candy and soda, eat at a fast-food restaurant and even skip breakfast,” says study author Leah Lipsky of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The research doesn’t prove that TV watching influences what kids eat, but strongly suggests a link between TV, snacking and a lack of exercise. Add questionable parenting to the mix and you have yet another contributing factor to America’s epidemic of childhood obesity. The average age of the children in the study was 13.
Another Link Between TV & Obesity From the “Wait, Didn’t We Know that Already?” department comes the news that kids who watch a lot of TV have poorer overall diets than kids whose exposure to television is limited. “The more TV you watch, the less likely you were to eat fruits and vegetables every day, and the more likely you were to eat things like candy and soda, eat at a fast-food restaurant and even skip breakfast,” says study author Leah Lipsky of the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The research doesn’t prove that TV watching influences what kids eat, but strongly suggests a link between TV, snacking and a lack of exercise. Add questionable parenting to the mix and you have yet another contributing factor to America’s epidemic of childhood obesity. The average age of the children in the study was 13.


 Smoking While Pregnant: Are Friends Actually Foes? Most people are aware that smoking and pregnancy don’t mix. Yet expectant mothers continue to puff away, or live in smoking environments. A recent study published in the journal Addictive Behaviors looked at some of the reasons this situation persists. It was no shock to find that nearly half of pregnant women who smoke had a partner who also smoked. It was a surprise, however, to find that women who had close friends that smoke were far more likely to smoke themselves. In fact, the influence of friends was actually higher than the influence of family members. The study, conducted by researchers at SUNY Buffalo from 2006 to 2011, will continue, and focus on generating data on the children of pregnant smokers.
Smoking While Pregnant: Are Friends Actually Foes? Most people are aware that smoking and pregnancy don’t mix. Yet expectant mothers continue to puff away, or live in smoking environments. A recent study published in the journal Addictive Behaviors looked at some of the reasons this situation persists. It was no shock to find that nearly half of pregnant women who smoke had a partner who also smoked. It was a surprise, however, to find that women who had close friends that smoke were far more likely to smoke themselves. In fact, the influence of friends was actually higher than the influence of family members. The study, conducted by researchers at SUNY Buffalo from 2006 to 2011, will continue, and focus on generating data on the children of pregnant smokers. Good News on Concussions If you happen to be a hockey fan, you know that NHL superstar Sidney Crosby nearly lost his entire season to a concussion. What finally helped him get back on the ice was the diagnosis and treatment of a soft-tissue neck injury that accompanied the concussion. This was no surprise to the doctors at the MMTR Health Clinic in Guelph, Ontario, which has been treating hockey concussions for years. They have found that many symptoms attributed to the lingering effects of a concussion actually correspond to specific neck muscles damaged at the time of the original injury. Once treatment is individualized and the muscles repaired, patients experience speedy postconcussive recoveries.
Good News on Concussions If you happen to be a hockey fan, you know that NHL superstar Sidney Crosby nearly lost his entire season to a concussion. What finally helped him get back on the ice was the diagnosis and treatment of a soft-tissue neck injury that accompanied the concussion. This was no surprise to the doctors at the MMTR Health Clinic in Guelph, Ontario, which has been treating hockey concussions for years. They have found that many symptoms attributed to the lingering effects of a concussion actually correspond to specific neck muscles damaged at the time of the original injury. Once treatment is individualized and the muscles repaired, patients experience speedy postconcussive recoveries. a Body Mass Index (BMI) of 18.5 or more. A media storm ensued, with critics of the law saying the government should aim its efforts on health as opposed to weight. Indeed, some models now disqualified are naturally skinny and completely healthy. Should they be prevented from earning a living without knowing whether they are actually unhealthy in some way? The Israeli government points to statistics that show 1 in 50 teenage girls suffers from an eating disorder, and stands by its position.
a Body Mass Index (BMI) of 18.5 or more. A media storm ensued, with critics of the law saying the government should aim its efforts on health as opposed to weight. Indeed, some models now disqualified are naturally skinny and completely healthy. Should they be prevented from earning a living without knowing whether they are actually unhealthy in some way? The Israeli government points to statistics that show 1 in 50 teenage girls suffers from an eating disorder, and stands by its position. Is There an Autism Epidemic? A March study released by the Centers for Disease Control and Prevention estimates that 1 in 88 children born in the U.S. suffers from a disorder on the autism spectrum. The last study estimated the ratio to be 1 in 110 and one done in 2002 suggests that the number of autistic children has doubled since then to around one million. Does this mean there is an “epidemic” of autism? Most doctors and researchers believe this is not the case. Instead, the numbers reflect better diagnostic screening tools and earlier detection. There is no “test” for autism, such as a blood test; it is detected through observing behavior of children typically around the age of eight. “One thing the data tells us with certainty,” says CDC Director Dr. Thomas Frieden, “is there are many children and families who need help.”
Is There an Autism Epidemic? A March study released by the Centers for Disease Control and Prevention estimates that 1 in 88 children born in the U.S. suffers from a disorder on the autism spectrum. The last study estimated the ratio to be 1 in 110 and one done in 2002 suggests that the number of autistic children has doubled since then to around one million. Does this mean there is an “epidemic” of autism? Most doctors and researchers believe this is not the case. Instead, the numbers reflect better diagnostic screening tools and earlier detection. There is no “test” for autism, such as a blood test; it is detected through observing behavior of children typically around the age of eight. “One thing the data tells us with certainty,” says CDC Director Dr. Thomas Frieden, “is there are many children and families who need help.”

 You may have heard some encouraging news over the holidays about the fight against HIV/AIDS. The United Nations announced that both AIDS-related deaths and new HIV infections have dropped to their lowest levels since the peak of the epidemic in the 1990s. Worldwide, new infections have dropped 21% since 1997 and deaths were down 21% since 2005. Researchers credit a combination of things for the dramatic improvements, including scientific breakthroughs, access to treatment, better political leadership and social change. The UN report also noted that HIV-infected individuals are also living longer.
You may have heard some encouraging news over the holidays about the fight against HIV/AIDS. The United Nations announced that both AIDS-related deaths and new HIV infections have dropped to their lowest levels since the peak of the epidemic in the 1990s. Worldwide, new infections have dropped 21% since 1997 and deaths were down 21% since 2005. Researchers credit a combination of things for the dramatic improvements, including scientific breakthroughs, access to treatment, better political leadership and social change. The UN report also noted that HIV-infected individuals are also living longer. abdominal cramping underscores the importance of catching colon cancer in its early stages. This individual, who was literally surrounded by doctors every day, put off a visit to his GP until the condition became unbearable. When he finally had it checked out, he was diagnosed with metastatic inoperable carcinoma of the colon. Colon cancer is the third leading cause of cancer-related death for both men and women. Yet it is 95 percent curable if diagnosed before symptoms arise. Most colorectal cancer begins as a non-cancerous (benign) adenoma or polyp (abnormal growth) that develops on the lining of the colon or rectum. Polyps can be removed to significantly reduce the risk of cancer.
abdominal cramping underscores the importance of catching colon cancer in its early stages. This individual, who was literally surrounded by doctors every day, put off a visit to his GP until the condition became unbearable. When he finally had it checked out, he was diagnosed with metastatic inoperable carcinoma of the colon. Colon cancer is the third leading cause of cancer-related death for both men and women. Yet it is 95 percent curable if diagnosed before symptoms arise. Most colorectal cancer begins as a non-cancerous (benign) adenoma or polyp (abnormal growth) that develops on the lining of the colon or rectum. Polyps can be removed to significantly reduce the risk of cancer. E-Shoppers Under the Influence One of the most unusual trends to emerge this past holiday season was a sharp rise in “drunk shopping.” Drunk shopping is exactly what it sounds like. People have a couple of drinks, go online, and start buying things they normally wouldn’t. E-tailers know this is happening. They can tell when someone orders 10 of something instead of one—they have impatiently clicked the BUY button too many times. Another sign is when shoppers botch selections from a drop-down menu, such as which state they live in.
E-Shoppers Under the Influence One of the most unusual trends to emerge this past holiday season was a sharp rise in “drunk shopping.” Drunk shopping is exactly what it sounds like. People have a couple of drinks, go online, and start buying things they normally wouldn’t. E-tailers know this is happening. They can tell when someone orders 10 of something instead of one—they have impatiently clicked the BUY button too many times. Another sign is when shoppers botch selections from a drop-down menu, such as which state they live in. risk of miscarriage, underweight birth, or diminished IQ for her baby. Doctors know to treat severe cases with hormone medication, but there is a growing debate about how to handle milder “gray-area” cases. Roughly a quarter of pregnant women receive a thyroid blood test whether they have symptoms or not. Testing lab Quest Diagnostics recently reported that about 15% of the expectant mothers it tested showed signs of an underactive thyroid, which surprised many. An underactive thyroid (aka hypothyroidism) slows body functions, causing such problems as fatigue, weight gain and depression.
risk of miscarriage, underweight birth, or diminished IQ for her baby. Doctors know to treat severe cases with hormone medication, but there is a growing debate about how to handle milder “gray-area” cases. Roughly a quarter of pregnant women receive a thyroid blood test whether they have symptoms or not. Testing lab Quest Diagnostics recently reported that about 15% of the expectant mothers it tested showed signs of an underactive thyroid, which surprised many. An underactive thyroid (aka hypothyroidism) slows body functions, causing such problems as fatigue, weight gain and depression. to protect themselves by staying slim and active, focusing on healthful, natural foods, and avoiding the disease-causing foods common in the standard American diet. According to Dr. Joel Fuhrman, author of Super Immunity, the keys to a cancer-resisting diet include getting your folic acid from green vegetables (as opposed to the synthetic type contained in multivitamins and prenatal vitamins); taking a daily dose of ground flaxseed (which contains estrogen-blocking lignans); eating your GOMBBS (greens, onions, mushrooms, beans, berries and seeds); minimizing the consumption of meat, fish and dairy products, and avoiding white flour and sugars.
to protect themselves by staying slim and active, focusing on healthful, natural foods, and avoiding the disease-causing foods common in the standard American diet. According to Dr. Joel Fuhrman, author of Super Immunity, the keys to a cancer-resisting diet include getting your folic acid from green vegetables (as opposed to the synthetic type contained in multivitamins and prenatal vitamins); taking a daily dose of ground flaxseed (which contains estrogen-blocking lignans); eating your GOMBBS (greens, onions, mushrooms, beans, berries and seeds); minimizing the consumption of meat, fish and dairy products, and avoiding white flour and sugars.
 Calderon, Ed. D—the museum’s Director of Science and curator of Generation Fit—gave EDGE a tantalizing sneak peek. Calderon calls it an exploratory space, and that it is. But here’s the clever part—as kids explore the interactive exhibits, lessons of healthy eating, the benefits of exercise and a profound awareness of their own bodies start to sink in.
Calderon, Ed. D—the museum’s Director of Science and curator of Generation Fit—gave EDGE a tantalizing sneak peek. Calderon calls it an exploratory space, and that it is. But here’s the clever part—as kids explore the interactive exhibits, lessons of healthy eating, the benefits of exercise and a profound awareness of their own bodies start to sink in. interactive display provides feedback on whether the selected meal is sufficiently balanced. It also provides alternative food choices. As you work your way around the exhibit hall, you’ll encounter the Label Decoder, Sugar Detective, Dollars and Scents, Know Your BMI, Exertainment and FIT Center (FIT is an acronym for frequency, intensity & time). You can probably make an educated guess at what each offers, and you’d be right. The key thing here is that Calderon (left) has seen to it that each section over-delivers. Two good things to know about Generation Fit. First, to avoid the chaos and disorder that sometimes diminish other interactive children’s exhibits, the Newark Museum will probably be time-ticketing the exhibit. This is a great idea. Call ahead to get details on this. Second, the crowded times for Generation Fit will probably be between noon and 2:00 pm. Plan accordingly.
interactive display provides feedback on whether the selected meal is sufficiently balanced. It also provides alternative food choices. As you work your way around the exhibit hall, you’ll encounter the Label Decoder, Sugar Detective, Dollars and Scents, Know Your BMI, Exertainment and FIT Center (FIT is an acronym for frequency, intensity & time). You can probably make an educated guess at what each offers, and you’d be right. The key thing here is that Calderon (left) has seen to it that each section over-delivers. Two good things to know about Generation Fit. First, to avoid the chaos and disorder that sometimes diminish other interactive children’s exhibits, the Newark Museum will probably be time-ticketing the exhibit. This is a great idea. Call ahead to get details on this. Second, the crowded times for Generation Fit will probably be between noon and 2:00 pm. Plan accordingly.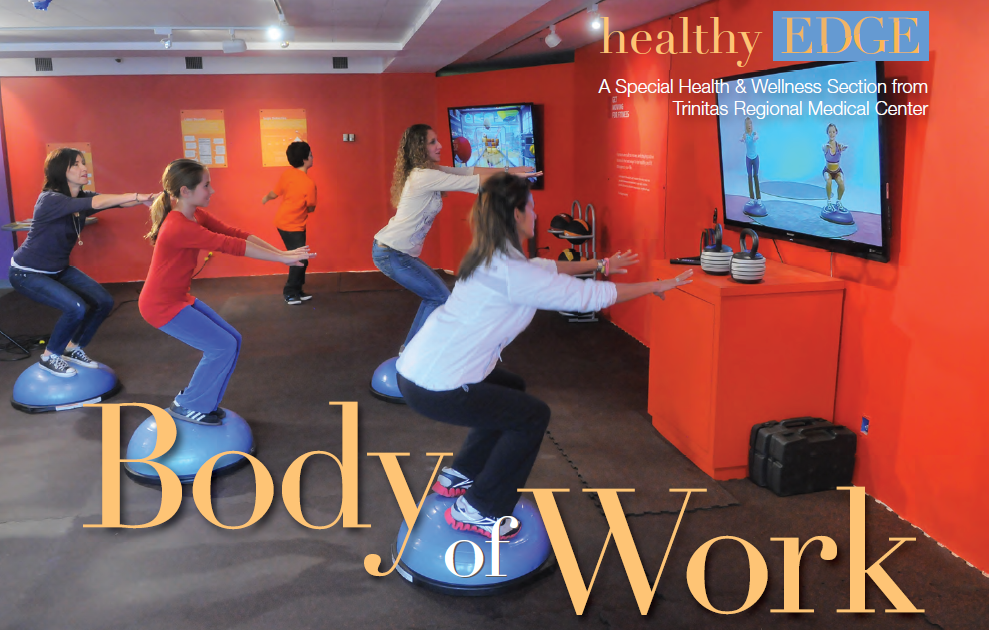
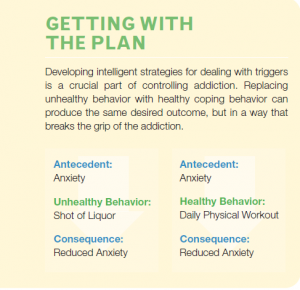 Goddard: The greater our ability to identify a trigger, the stronger we become at overcoming an addiction. Trigger awareness can help us to substitute a behavior that does not injure our health or quality of life. When we can identify our triggers it is possible to stop the negative action before it takes us over. Writing down triggers can be a first step in overcoming addictions. Sometimes we are able to overcome an addiction on our own, but sometimes it is critical to get help from a therapist, clinic or professionals that specialize in addiction.
Goddard: The greater our ability to identify a trigger, the stronger we become at overcoming an addiction. Trigger awareness can help us to substitute a behavior that does not injure our health or quality of life. When we can identify our triggers it is possible to stop the negative action before it takes us over. Writing down triggers can be a first step in overcoming addictions. Sometimes we are able to overcome an addiction on our own, but sometimes it is critical to get help from a therapist, clinic or professionals that specialize in addiction.





 health to patients who in the past might have been rejected as a bariatric surgical candidate. Higher-weight patients are more challenging to operate on because their body structure places limitations on conventional laparoscopic instruments. The da Vinci diminishes the problem by giving the surgeon greater control and maneuverability. The da Vinci is also good for revisional surgeries, where a bariatric patient needs a procedure redone, or must switch from a band to a bypass. Where will robotics take bariatric surgeons in the future? Anywhere they want. Indeed, seated inside the da Vinci pod and controlling the camera, a surgeon at Trinitas could theoretically perform a bypass on anyone, anywhere. This could have interesting implications for remote parts of our own country, where obesity is epidemic and trained surgeons are few.
health to patients who in the past might have been rejected as a bariatric surgical candidate. Higher-weight patients are more challenging to operate on because their body structure places limitations on conventional laparoscopic instruments. The da Vinci diminishes the problem by giving the surgeon greater control and maneuverability. The da Vinci is also good for revisional surgeries, where a bariatric patient needs a procedure redone, or must switch from a band to a bypass. Where will robotics take bariatric surgeons in the future? Anywhere they want. Indeed, seated inside the da Vinci pod and controlling the camera, a surgeon at Trinitas could theoretically perform a bypass on anyone, anywhere. This could have interesting implications for remote parts of our own country, where obesity is epidemic and trained surgeons are few. During a normal laparoscopic procedure, an assistant handles the camera. This gives surgeons more control over where their eyes are trained. Imagine wanting to look at something and having someone else controlling your eyes.” In a robotic procedure, the surgeon is removed from the side of the operating table. The standard operating team is around the patient. Above the patient cart is the robotic arm. There is one surgical assistant on hand to perform tasks like retracting and stapling.
During a normal laparoscopic procedure, an assistant handles the camera. This gives surgeons more control over where their eyes are trained. Imagine wanting to look at something and having someone else controlling your eyes.” In a robotic procedure, the surgeon is removed from the side of the operating table. The standard operating team is around the patient. Above the patient cart is the robotic arm. There is one surgical assistant on hand to perform tasks like retracting and stapling.
 The term “guesswork” is not a particularly comforting one for early-stage breast cancer patients. Once a lumpectomy has been performed, the diagnosis confirmed and radiotherapy initiated, women want to know that radiation is going to the right place. Now they can check the doctor’s work for themselves. In June, Trinitas Regional Medical Center became the first cancer treatment facility in the state to offer breast cancer patients a radiotherapy technology called AccuBoost. Developed by Nucletron, a company headquartered in the Netherlands, AccuBoost enables doctors and patients to actually see the area receiving radiation treatment as it receives it. In other words, no guesswork. The system images the site where cancer was removed so that the surrounding breast tissue can be treated more accurately with boost-dose targeting. “AccuBoost utilizes real-time mammography to localize the treatment,” says Clarissa Henson, MD, Chair of Radiation Oncology at Trinitas (above). “This technology is far superior to the current standard of care treatment. On average, only 51 percent of the treatment area receives 90 percent of the dose when using the current standard of care. With AccuBoost, targeting is improved and a more effective dose of radiation is delivered to the tumor site.” With AccuBoost, a technician can position the applicator so that it delivers the therapeutic dose accurately and reliably, with limited radiation exposure to the skin. The dose is uniform over the portion of the breast that is being irradiated, which reduces unnecessary exposure of healthy tissue to radiation and enables patients to retain more undamaged tissue.
The term “guesswork” is not a particularly comforting one for early-stage breast cancer patients. Once a lumpectomy has been performed, the diagnosis confirmed and radiotherapy initiated, women want to know that radiation is going to the right place. Now they can check the doctor’s work for themselves. In June, Trinitas Regional Medical Center became the first cancer treatment facility in the state to offer breast cancer patients a radiotherapy technology called AccuBoost. Developed by Nucletron, a company headquartered in the Netherlands, AccuBoost enables doctors and patients to actually see the area receiving radiation treatment as it receives it. In other words, no guesswork. The system images the site where cancer was removed so that the surrounding breast tissue can be treated more accurately with boost-dose targeting. “AccuBoost utilizes real-time mammography to localize the treatment,” says Clarissa Henson, MD, Chair of Radiation Oncology at Trinitas (above). “This technology is far superior to the current standard of care treatment. On average, only 51 percent of the treatment area receives 90 percent of the dose when using the current standard of care. With AccuBoost, targeting is improved and a more effective dose of radiation is delivered to the tumor site.” With AccuBoost, a technician can position the applicator so that it delivers the therapeutic dose accurately and reliably, with limited radiation exposure to the skin. The dose is uniform over the portion of the breast that is being irradiated, which reduces unnecessary exposure of healthy tissue to radiation and enables patients to retain more undamaged tissue. st traumatic for any woman,” says Dr. Henson. “Being able to see treatment as it is delivered through this new technology helps patients be informed and involved in their care.” “Trinitas was the first cancer treatment center in New Jersey to offer Rapid Arc radiotherapy technology and now we are the first with AccuBoost,” adds TRMC President and CEO Gary S. Horan (right). “It’s another clear example of why Trinitas Comprehensive Cancer Center is a regional leader in cancer care.”
st traumatic for any woman,” says Dr. Henson. “Being able to see treatment as it is delivered through this new technology helps patients be informed and involved in their care.” “Trinitas was the first cancer treatment center in New Jersey to offer Rapid Arc radiotherapy technology and now we are the first with AccuBoost,” adds TRMC President and CEO Gary S. Horan (right). “It’s another clear example of why Trinitas Comprehensive Cancer Center is a regional leader in cancer care.”