By pulling out all the stops, have we inadvertently pulled the rug out from under our best young athletes?
The intense pressure experienced by athletes at the top of their sport and the apex of their abilities is nothing new. It comes with the territory and is amplified exponentially when the stakes are highest, the competition is fiercest and the whole world is watching. The best of the best separate themselves from the pack at these make-or-break moments, digging deep and finding ways to meet or exceed the fantastic expectations heaped upon them. Until, one day, they can’t. Or don’t. Or won’t.
And we are stunned.
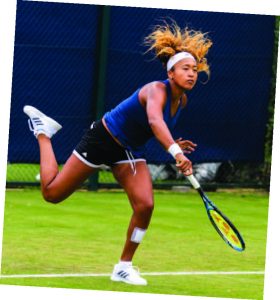
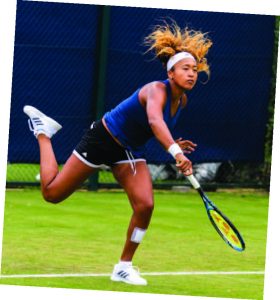
We know that Simone Biles and Naomi Osaka are made of flesh and blood and sinew—they may be marvels of sport, but they are not part of the Marvel Universe. Yet we don’t really understand what nudges them off the rails, do we? Biles opted out of the Olympic all-around gymnastics competition when her internal wiring betrayed her. Osaka took a mental-health vacation from tennis at the height of the spring/summer season. More surprising than their decisions—and more alarming than some of the public criticism they shouldered—is the eye-opening realization that they are not the exception in sports. They are actually the rule.
An Unexpected Twist
On July 27, 2021, inside the physically crowd-less Ariake Gymnastics Centre, Simone Biles (right), leading her team into the Tokyo Olympics finals against the Russian contender

Fernando Frazão/Agência Brasil Fotografias
s, elevated off the mat with her usual power and grace…and failed to perform the 2 ½ rotation vault she had nailed countless times. She scored only 13.766 points, putting Team USA behind in the competition for the first time in almost a decade. Her failure on her sport’s biggest stage left television commentators stunned and her teammates speechless. What Biles did next shocked the world of competitive sports: She publicly withdrew from the Olympic finals, citing non-injury related mental health issues.
Peter Menzel
“I just felt like it would be a little bit better to take a back seat, work on my mindfulness,” Biles told reporters. “I just need to let the girls do it and focus on myself.”
Sian L. Beilock, the president of Barnard College and a cognitive scientist told The New York Times, “I applaud the fact [Simone Biles] was able to ascertain that she wasn’t in the right state of mind and step back. What a hard thing to do. There was so much pressure to continue. And she was able to find the strength to say, ‘No, this is not right.’”
Biles later credited Naomi Osaka (left)—who withdrew from the 2021 French Opens to focus on her own mental health and depression—as providing the motivation and courage she needed to put her own mental health first. Osaka had disclosed her decision to withdraw during the French Open on Twitter; she had been unable to manage her mental health, depression and press conference anxiety ever since her controversial 2018 US Open finals victory over Serena Williams, during which she endured the jeers and boos of a crowd that favored Williams.
Both Biles and Osaka had their critics, of course, some quite harsh. However, they received an outpouring of support from fellow elite-level athletes, who understood the immense, round-the-clock pressure to which they are subjected. Knowledgeable fans by and large echoed this support, as did most in the media. The two young champions compete in sports that favor youth physically, but demand a level of mental maturity that appeared to be beyond their grasp. And it just got to be too much.
An Epidemic
The thing is, Simone Biles and Naomi Osaka are not one-offs. Indeed, every year, countless young elite-level athletes on the fast track to stardom—many still young teens or pre-teens—are overwhelmed by pressure and expectations placed upon them by parents, coaches, fans and friends, and begin to hate the thing they loved the most. Unless you know them, or they are your kids, their stories go untold. Most youth sports programs, in fact, are set up to cull out the physically fragile or easily upended and push the rest ever forward. Although the survivors may gain confidence in their growing skills, the pressure cooker only grows more intense as they near the top of their sport.
Past a certain level, athletes will acknowledge that this unrelenting pressure—as Billie Jean King once said—is a “privilege.” But how do you explain the meltdown of a superstar? And, more importantly, what does that tell us about how young athletes are being raised today?
Studies done on the mental health issues of elite athletes give us the same picture over and over, and it’s kind of stunning. A study on NCAA Division I athletes found that 23.6% of the individuals included in the study met the clinically relevant level of depressive symptoms, with female athletes being nearly twice as likely as male athletes to experience depression. The prevalence rate for American college students, if you’re wondering, is between 7% and 9% depending on the study.
A UK study found the prevalence of mental health issues among elite athletes to be 47.8% for depression and anxiety and 26.8% for signs of distress. A similar study in Australia found the prevalence rate for mental health disorders overall to be 46.4%. A study in Sweden revealed that lifetime prevalence of mental health problems in elite athletes was 51.7% (females 58.2%, males 42.3%).
“The professional consensus is that the incidence of anxiety and depression among scholastic athletes has increased over the past 10 to 15 years,” says Marshall Mintz, a New Jersey-based sports psychologist who has worked with teenagers for three decades.
Isabella and Vinny

Swimming World Magazine
The story of Isabella [last name withheld], a prodigal lacrosse player who started to play when she was in first grade, is not unusual. Excelling at the game from the start, she gave up on other sports she enjoyed, including basketball and soccer, to optimize her shot at a college scholarship. Sure enough, Isabella earned a full ride from an elite college during her sophomore year in high school. What she loved most about lacrosse was the attention it garnered in her hometown. Everyone was rooting for her, and that made her play and practice the sport even harder. That summer, Isabella tore her ACL and was unable to play for eight months.
“It was my worst year ever,” she recalls. “I’d grown up playing lacrosse, and I had no other hobbies. So when you don’t have it, you’re like, What am I going to do?”
Like so many other young athletes, she had been pushed and pressured by her peers, her parents and coaches to focus solely on the sport she was good at—naturally, with love and caring and unqualified support. She practiced day in and day out, cultivated an athletic identity and, in the end, all this over-practice made her more vulnerable to her knee injury. With nothing else to occupy her mind, and the sight of her peers moving ahead with their lacrosse tournaments while she had to take up painful physical therapy, Isabella soon developed an eating disorder. In the end, she chose to give up on the sport to which she had devoted a decade of her young life, deciding instead to pursue a university degree and a career outside lacrosse.
Isabella’s story is hardly unique. Thanks to the changing nature of youth sports, there is an Isabella in almost every town in the country. In 2018, the American Academy of Orthopaedic Surgeons (AAOS) cited two independent studies that strongly suggested that an intense, year-round focus on one sport leads to a much higher risk of burnout and injury in young athletes, as they routinely spend excessive hours per week training. “Youth sports has experienced a paradigm shift over the past 15 to 20 years,” the AAOS noted. “Gone are the days filled with pick-up basketball games and free play. Kids are increasingly specializing in sports.”
Vinny Marciano, a swimming prodigy from New Jersey, was considered by Swimming World and other authorities in the sport to be one of America’s best young swimmers in the run-up to the 2016 Olympic Games. He was the New Jersey 100-yard freestyle champion, and the 2015-16 All Daily Swimmer of the Year, propelling Randolph High School to win the team title despite suffering tendinitis earlier that same year. He missed making the 2016 Olympic by just 0.27 seconds in the 100-meter backstroke. A year later, Marciano all but disappeared from the world of competitive swimming.
In a sport where obscurity and glory are often separated by mere fractions of a second, Marciano knew what he had to do. After failing in the Olympic trials, he joined an even more intense swimming club 90 minutes from home, where he had to put in three-hour practice sessions straight after school, stay overnight with a teammate, get up early and get through two more hours of practice before arriving late to school the next day. For six miserable months, these were his Mondays, Wednesdays and Fridays, with additional solo sets by a coach at a local YMCA. His grades tanked and, finally, he told his parents he did not want to keep going like this.
According to Jay Coakley, a leading sports sociologist and author of Sports in Society: Issues and Controversies, parental pressure doesn’t need to be explicit and heavy-handed in order to push a young athlete past his or her comfort level. Instead, just the child’s awareness of the time and money sacrificed by their parents is enough pressure to make the child keep playing long past enjoyment.
In the end, Marciano completely gave up on competitive swimming to get away from the misery of always trying to climb up a never-ending ladder. He found challenge and enjoyment in a much more leisurely sport: rock climbing. Had it not been for the intense training pressure felt by Marciano—a swimming prodigy by most accounts—after coming up short in Olympic qualifying, the swimming world might have witnessed another Michael Phelps.
Is This PTSD?
The Oxford English Dictionary defines post-traumatic stress syndrome (PTSD) as a condition of persistent mental and emotional stress occurring as a result of injury or severe psychological shock. While the PTSD symptoms in athletes with traumatic injuries, such as a concussion or a torn ACL, are well-studied, that is not the case for a very large number of elite athletes who are subject to emotional and psychological trauma in the form of bullying, humiliation, body shaming, being belittled in front of teammates by coaches or any other similar traumatizing emotional experience.
Former Olympic martial artist and (now) sports psychologist Caroline Anderson brings some personal insight into her new profession. “In my private practice,
I see a lot of athletes—many of them quite young—who have been traumatized in some way as a result of being an athlete and their involvement in sport,” she says, adding that, in addition to serious injury, trauma ranges from conflict with coaches, teammates and sporting bodies to bullying, politics, unfair selection processes and the embarrassment and shame that accompanies less-than-expected performance.
In some cases, the source of PTSD symptoms can be something entirely separate from the performance pressure of an athlete’s chosen sport. Simone Biles was among the scores of U.S. gymnasts sexually abused by team doctor Larry Nasser. During testimony before a Senate Judiciary Committee, Biles was reduced to tears when discussing her experience and its long-term aftermath.
“I can assure you,“ she told the committee, “that the impacts of this man’s abuse are never over or forgotten.”
PTSD symptoms affect a significant percentage of young athletes in some way or form, and for those without proper support, they linger long past the trauma. What matters most is having good support and people who actually understand their struggles. Perhaps that explains why the prevalence of PTSD appears to be much lower among traditional team sports athletes.
Basketball Hall of Famer Magic Johnson, who decades ago said, “Ask not what your teammates can do for you…ask what you can do for your teammates,” may have been on to something. Team sports inherently provide a much bigger support net for the mental health of young athletes who devote themselves to a single sport. Often, they sacrifice their social lives in their quest for excellence. In lieu of close friendships, however, they have teammates that rely upon one another for mental support.
Though not a perfect answer, it’s an improvement over the situation individual-sport athletes like Vinny Marciano live with, as they get stuck in a Sisyphean cycle of chasing perfection and dealing with often overwhelming pressure to always perform better. Indeed, a 2019 study found that individual-sport athletes are more likely to report anxiety and depression, and tend to play less “for fun” and more for goals than team-based sports athletes.
The culture of elite-level athletics, from teen sports to the pros, places a high value on mental resilience. Ironically, that culture has also been largely apathetic to the mental health needs of athletes until relatively recently. USC Sports Psychologist Robin Scholefield may have put it best when she observed that the whole healthy person is the most consistent peak performer. “If you’re not right with yourself,” she insists, “you’re not going to be okay as an athlete.”
Michael Phelps is one of the few elite-level male athletes to step forward and talk about his mental health issues, including a struggle with depression that only worsened during the pandemic. He encourages others to speak out, as he did prior to the 2016 Olympics. “It wasn’t easy to admit I wasn’t perfect,” he says. “But opening up took a huge weight off my back.”

Agência Brasil Fotografias
In 2021, three major college sports conferences—the Atlantic Coast Conference, Big Ten and Pac-12—launched a joint initiative called Teammates for Mental Health. So things are changing. Of course, the hard work still begins at home.
As a parent or as a coach, remember that not a single person has ever succeeded by blindly burning themselves out on a sport that makes them miserable. It is healthy for children to have sports dreams, but what is equally important is to make sure that the child learns other skills to fall back on in case their dreams are not achieved or are not all that they wanted them to be.
Multiple generations are responsible for creating the mess of mental health issues that can consume young elite-level athletes. Perhaps this generation of athletes, with their public platforms and social media followings, will follow the lead of Simone Biles, Naomi Osaka and a handful of others in making the world of sports more in tune with the mental health needs of athletes. Hopefully, their willingness to open up on the subject, to the possible detriment of their image and the value of their “brand,” triggers the kind of culture change that will swing the mental-health pendulum back in favor of the next generation of young, high-performance athletes. EDGE
Editor’s Note: Chuka Erike has been involved in the sports industry since his college days. In 2016, while working for the NBA, Chuka won the league’s Community Assist Award. During a career in sports that stretches back more than 15 years, he has devoted himself to working with young athletes who face high pressure and unrealistic expectations. He recently mentored Joey Spallina, the nation’s top-ranked lacrosse recruit, who is headed for Syracuse University in the fall.



 Editor’s Note:
Editor’s Note: 




 In May 2023, the Brookings Institution released findings on ARRIVE Together, looking at data from more than 300 calls between December 2021 and January of this year—including critically important Officer Narrative Reports. Dr. Rashawn Ray, a Senior Fellow in Governance Studies, joined New Jersey Attorney General Matthew Platkin on a panel that included Lisa Dressner of RWJBarnabas Health, who is Vice President of the Department of Behavioral Health at Trinitas.
In May 2023, the Brookings Institution released findings on ARRIVE Together, looking at data from more than 300 calls between December 2021 and January of this year—including critically important Officer Narrative Reports. Dr. Rashawn Ray, a Senior Fellow in Governance Studies, joined New Jersey Attorney General Matthew Platkin on a panel that included Lisa Dressner of RWJBarnabas Health, who is Vice President of the Department of Behavioral Health at Trinitas.




 As with any screening test, there are risks and benefits, Dr. Li adds.
As with any screening test, there are risks and benefits, Dr. Li adds.















 Over the past year, chances are that you have heard more facts and figures about vaccines than in all of the other years of your lifetime combined. Yet while we have all become intimately familiar with the COVID-19 vaccine, there is another vaccine on the market, which—in any other year—would have been the real headline-maker. Last year, the World Health Organization (WHO) announced that it had approved use of the first-ever vaccine that is effective against malaria, a mosquito-borne disease that can kill within 24 hours of its flu-like symptoms appearing.
Over the past year, chances are that you have heard more facts and figures about vaccines than in all of the other years of your lifetime combined. Yet while we have all become intimately familiar with the COVID-19 vaccine, there is another vaccine on the market, which—in any other year—would have been the real headline-maker. Last year, the World Health Organization (WHO) announced that it had approved use of the first-ever vaccine that is effective against malaria, a mosquito-borne disease that can kill within 24 hours of its flu-like symptoms appearing. The new vaccine, which has been recommended for children five years old and younger, marks a significant step in an effort to conquer malaria that has seen worldwide deaths drop by 60% in the last two decades, and the number of cases cut nearly in half. Unfortunately, progress reached a kind of plateau around 2015 and the numbers have remained more or less constant since then. The recent breakthrough, which activates the immune system to battle the malaria pathogen, owes much to the work done in speeding COVID vaccines to market.
The new vaccine, which has been recommended for children five years old and younger, marks a significant step in an effort to conquer malaria that has seen worldwide deaths drop by 60% in the last two decades, and the number of cases cut nearly in half. Unfortunately, progress reached a kind of plateau around 2015 and the numbers have remained more or less constant since then. The recent breakthrough, which activates the immune system to battle the malaria pathogen, owes much to the work done in speeding COVID vaccines to market.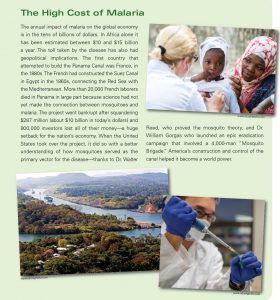 Impact on the Home Front
Impact on the Home Front 





















 caffeinated beverages, cigarettes, chocolate—can cause sleep problems. If the room isn’t dark enough, or if you leave a TV on, that can interfere with sleep. Engaging in some sort of stimulating activity, like an office conference, an argument or a workout, can make it hard to fall asleep.” Even something that’s often considered a sleep aid—we’re talking nightcap here—can backfire. “Alcohol may make you drowsy enough to fall asleep, but you’ll wake up again in a few hours,” explains Cheryl Krempa, RPh, MBA, Director of the Pharmacy at Trinitas.
caffeinated beverages, cigarettes, chocolate—can cause sleep problems. If the room isn’t dark enough, or if you leave a TV on, that can interfere with sleep. Engaging in some sort of stimulating activity, like an office conference, an argument or a workout, can make it hard to fall asleep.” Even something that’s often considered a sleep aid—we’re talking nightcap here—can backfire. “Alcohol may make you drowsy enough to fall asleep, but you’ll wake up again in a few hours,” explains Cheryl Krempa, RPh, MBA, Director of the Pharmacy at Trinitas.

 arrangements are made. For those who cannot (or will not) leave home to participate in a study, Dr. Garg proposes an alternative possibility: an at-home sleep study, using a new portable device that collects the same useful data. Success stories are hardly few and far between at Trinitas Comprehensive Sleep Disorders Center. On the contrary, the center conducted nearly 1,500 studies in 2012, including adults and children. One of Dr. Garg’s favorite stories concerns an eight-year-old boy, who was prescribed ADHD medication after meeting with a psychiatrist and pediatrician for hyperactivity and inattention in school.
arrangements are made. For those who cannot (or will not) leave home to participate in a study, Dr. Garg proposes an alternative possibility: an at-home sleep study, using a new portable device that collects the same useful data. Success stories are hardly few and far between at Trinitas Comprehensive Sleep Disorders Center. On the contrary, the center conducted nearly 1,500 studies in 2012, including adults and children. One of Dr. Garg’s favorite stories concerns an eight-year-old boy, who was prescribed ADHD medication after meeting with a psychiatrist and pediatrician for hyperactivity and inattention in school.
 sure you are on-track to reach your goals.
sure you are on-track to reach your goals.
 Editor’s Note: Gerontologist Alexis Abramson, PhD appears frequently as an on-air expert for NBC’s Today show, and also on CNN, CBS and MSNBC. Her commitment to baby boomers and mature adults has been featured in TIME, Forbes, The Wall Street Journal, People and other national publications. To see more of her thoughts on aging gracefully (and intelligently), log onto alexisabramson.com.
Editor’s Note: Gerontologist Alexis Abramson, PhD appears frequently as an on-air expert for NBC’s Today show, and also on CNN, CBS and MSNBC. Her commitment to baby boomers and mature adults has been featured in TIME, Forbes, The Wall Street Journal, People and other national publications. To see more of her thoughts on aging gracefully (and intelligently), log onto alexisabramson.com.
 Flip-Flopping in the Classroom The back-to-school season always holds some surprises for educators, kids and parents. This year, many noticed a rise in foot pain among returning students. The popularity of cheap, stylish flip-flops has more than a little to do with this, according to the American College of Foot and Ankle Surgeons. Right into the mid-teens, kids have new bone growing in their heels. Flip-flops offer no support or cushioning for this part of the foot, and summer-long repetitive stress can manifest itself in pain and injuries once students switch back to traditional school footwear. If your child is experiencing pain, it’s important to explore an immediate remedy—stretching exercises, ice massage, anti-inflammatory medications, and custom or over-the-counter shoe inserts are certainly worth exploring. Obviously, if the pain worsens or persists, a visit to the podiatrist is called for.
Flip-Flopping in the Classroom The back-to-school season always holds some surprises for educators, kids and parents. This year, many noticed a rise in foot pain among returning students. The popularity of cheap, stylish flip-flops has more than a little to do with this, according to the American College of Foot and Ankle Surgeons. Right into the mid-teens, kids have new bone growing in their heels. Flip-flops offer no support or cushioning for this part of the foot, and summer-long repetitive stress can manifest itself in pain and injuries once students switch back to traditional school footwear. If your child is experiencing pain, it’s important to explore an immediate remedy—stretching exercises, ice massage, anti-inflammatory medications, and custom or over-the-counter shoe inserts are certainly worth exploring. Obviously, if the pain worsens or persists, a visit to the podiatrist is called for. Follow-Up on NYC Soda Ban New York’s short-lived soda ban spurred a slew of studies on the actual impact of obesity-focused legislation. A recent article published in the American Journal of Agricultural Economics suggests that strategies such as taxing sugary beverages would not reduce obesity, because consumers would simply switch to un-taxed options. Public health advocates have posited that higher prices would deter unhealthy food purchases. But according to research economists, that simply isn’t the case. In New York, a court ruled that the Board of Health exceeded its authority in instituting the ban, which was pushed by Mayor Michael Bloomberg. Among the criticisms of an “obesity tax” is that it would target lower-income consumers who tend to buy more high-calorie foods and beverages, and thus would be a regressive tax. Even so, the search for a “social solution” will continue; more than a third of U.S. adults, and one in six children, are technically obese. The medical costs associated with obesity are between $125 and $150 billion a year.
Follow-Up on NYC Soda Ban New York’s short-lived soda ban spurred a slew of studies on the actual impact of obesity-focused legislation. A recent article published in the American Journal of Agricultural Economics suggests that strategies such as taxing sugary beverages would not reduce obesity, because consumers would simply switch to un-taxed options. Public health advocates have posited that higher prices would deter unhealthy food purchases. But according to research economists, that simply isn’t the case. In New York, a court ruled that the Board of Health exceeded its authority in instituting the ban, which was pushed by Mayor Michael Bloomberg. Among the criticisms of an “obesity tax” is that it would target lower-income consumers who tend to buy more high-calorie foods and beverages, and thus would be a regressive tax. Even so, the search for a “social solution” will continue; more than a third of U.S. adults, and one in six children, are technically obese. The medical costs associated with obesity are between $125 and $150 billion a year. Drug Wonder Downunder A pair of Australian medical researchers have been recognized for their breakthrough work with Duchenne Muscular Dystrophy, a condition caused by mutations in the dystrophin gene on the X chromosome—which means it mostly affects boys. DMD patients are wheelchair-dependent by age 12 and often don’t survive past their early 20s. The researchers have developed a drug that works by skipping over the faulty part of the gene, producing a functional version of the protein dystrophin. This protein stabilizes the muscle fiber during muscle contraction. Without dystrophin, muscle fibers are replaced by scar tissue. In clinical trials, boys on the drugs have been walking up hills, operating pedal cars and whistling after 90 weeks. “It is extremely exciting to see that genetic testing is finally coming to the forefront of clinical medicine,” says Dr. Kevin Lukenda, Chairman of TRMC’s Family Medicine Department. “For years, this information was limited to research and academia. With a simple swab of a patient’s saliva in my office, we can detect over 30 possible genetic mutations within an individual’s DNA. This is the future of early diagnoses and treatment in clinical medicine.”
Drug Wonder Downunder A pair of Australian medical researchers have been recognized for their breakthrough work with Duchenne Muscular Dystrophy, a condition caused by mutations in the dystrophin gene on the X chromosome—which means it mostly affects boys. DMD patients are wheelchair-dependent by age 12 and often don’t survive past their early 20s. The researchers have developed a drug that works by skipping over the faulty part of the gene, producing a functional version of the protein dystrophin. This protein stabilizes the muscle fiber during muscle contraction. Without dystrophin, muscle fibers are replaced by scar tissue. In clinical trials, boys on the drugs have been walking up hills, operating pedal cars and whistling after 90 weeks. “It is extremely exciting to see that genetic testing is finally coming to the forefront of clinical medicine,” says Dr. Kevin Lukenda, Chairman of TRMC’s Family Medicine Department. “For years, this information was limited to research and academia. With a simple swab of a patient’s saliva in my office, we can detect over 30 possible genetic mutations within an individual’s DNA. This is the future of early diagnoses and treatment in clinical medicine.” You Snooze, You Lose Don’t lose sleep over junk food purchases. Seriously, don’t. A new study shows that lack of sleep can lead people to buy more food—and more high-calorie items— when they shop. Researchers gave 14 normal-weight men a budget of $50 and instructed them to purchase as much as they could out of a possible 40 food items, which included 20 high-calorie and 20 low-calorie foods. They conducted this exercise after a night of sleep deprivation and again after a good night’s sleep. They bought 18 percent more food— and 9 percent more calories—after a night of sleep deprivation. “Another recent study showed tha
You Snooze, You Lose Don’t lose sleep over junk food purchases. Seriously, don’t. A new study shows that lack of sleep can lead people to buy more food—and more high-calorie items— when they shop. Researchers gave 14 normal-weight men a budget of $50 and instructed them to purchase as much as they could out of a possible 40 food items, which included 20 high-calorie and 20 low-calorie foods. They conducted this exercise after a night of sleep deprivation and again after a good night’s sleep. They bought 18 percent more food— and 9 percent more calories—after a night of sleep deprivation. “Another recent study showed tha t the pleasure centers of the brain were activated more when sleep-deprived people looked at pictures of junk food,” adds Dr. Vipin Garg, Director of the Trinitas Comprehensive Sleep Disorders Center. “Lack of sleep can prevent the brain from making an intelligent decision regarding healthy food choices. Getting enough quality sleep can help weight control by allowing people to make proper nutritional decisions and also provide energy to exercise to achieve better overall health.” There are plans in the works for follow-up studies to see how sleep deprivation affects other buying decisions.
t the pleasure centers of the brain were activated more when sleep-deprived people looked at pictures of junk food,” adds Dr. Vipin Garg, Director of the Trinitas Comprehensive Sleep Disorders Center. “Lack of sleep can prevent the brain from making an intelligent decision regarding healthy food choices. Getting enough quality sleep can help weight control by allowing people to make proper nutritional decisions and also provide energy to exercise to achieve better overall health.” There are plans in the works for follow-up studies to see how sleep deprivation affects other buying decisions. Word of Mouth Unreliable Where Strokes are Concerned So what’s the deal with the “Crooked Tongue” story making the rounds on social media? According to countless emails and Facebook postings, a woman who was suffering from a stroke but didn’t exhibit the typical symptoms was diagnosed by an alert ER physician who asked her to stick out her tongue. When she did so, and her tongue presented to one side rather than straight out, he was able to correctly diagnose the stroke and save his patient’s life. Is the “crooked tongue” technique a reliable way to diagnose stroke? According to Dr. John D’Angelo, Chairman of Trinitas Regional Medical Center’s Emergency Department, the story has all the earmarks of an urban legend. “I can find no reference to this suggestion from any reliable source, such as the Heart and Stroke Foundation, the American Heart Association or the National Institute of Neurological Disorders and Stroke,” he says. “Lingual deviation can indicate a host of issues that are typically associated with a tumor or other type of lesion. So a crooked tongue is a sign that something is wrong, but it’s not a reliable sign you are having a stroke.” The T in the American Stroke Assoc
Word of Mouth Unreliable Where Strokes are Concerned So what’s the deal with the “Crooked Tongue” story making the rounds on social media? According to countless emails and Facebook postings, a woman who was suffering from a stroke but didn’t exhibit the typical symptoms was diagnosed by an alert ER physician who asked her to stick out her tongue. When she did so, and her tongue presented to one side rather than straight out, he was able to correctly diagnose the stroke and save his patient’s life. Is the “crooked tongue” technique a reliable way to diagnose stroke? According to Dr. John D’Angelo, Chairman of Trinitas Regional Medical Center’s Emergency Department, the story has all the earmarks of an urban legend. “I can find no reference to this suggestion from any reliable source, such as the Heart and Stroke Foundation, the American Heart Association or the National Institute of Neurological Disorders and Stroke,” he says. “Lingual deviation can indicate a host of issues that are typically associated with a tumor or other type of lesion. So a crooked tongue is a sign that something is wrong, but it’s not a reliable sign you are having a stroke.” The T in the American Stroke Assoc
 promise for a more effective treatment of Type 2 Diabetes, which currently affects more than 25 million Americans. In the Harvard study, Belatrophin caused mice to produce insulin-secreting pancreatic beta cells at up to 30 times the normal rate. The new cells produce insulin only when called upon by the body. This offers the potential for natural regulation of insulin, as well as a reduction in the complications associated with diabetes. There is hope that this treatment may also have an impact on juvenile diabetes. It could eventually mean that instead of taking insulin injections three times a day, you might take an injection of this hormone once a week or once a month or—in the best case—maybe even once a year, explains Doug Melton, one of the researchers. “This new hormone offers optimism for researchers lo
promise for a more effective treatment of Type 2 Diabetes, which currently affects more than 25 million Americans. In the Harvard study, Belatrophin caused mice to produce insulin-secreting pancreatic beta cells at up to 30 times the normal rate. The new cells produce insulin only when called upon by the body. This offers the potential for natural regulation of insulin, as well as a reduction in the complications associated with diabetes. There is hope that this treatment may also have an impact on juvenile diabetes. It could eventually mean that instead of taking insulin injections three times a day, you might take an injection of this hormone once a week or once a month or—in the best case—maybe even once a year, explains Doug Melton, one of the researchers. “This new hormone offers optimism for researchers lo
 University of Oregon’s Department of Psychology, learning meditation techniques makes it easier for smokers to taper off. Mindful Meditation—a technique that encourages people to relax, focus on the current moment and “go with the flow” of thoughts and sensation—has already been shown to have a positive impact on cold and flu, hot flashes and irritable bowel syndrome. In the Oregon study, 60 people received five hours of either relaxation training or Mindful Meditation training. Among the smokers in the study, there was no difference in the amount the relaxation group smoked. However, the smokers in the meditation group had cut back by 60 percent. Researchers admit that the smoking findings are surprising, and caution that the study was very small. Also, the participants were all college students. On the other hand, none of the subjects were told they were taking part in a smoking study. And the Oregon study found that the brains of the smokers who learned meditation techniques were more active in an area linked to self-control. More work in this area is warranted.
University of Oregon’s Department of Psychology, learning meditation techniques makes it easier for smokers to taper off. Mindful Meditation—a technique that encourages people to relax, focus on the current moment and “go with the flow” of thoughts and sensation—has already been shown to have a positive impact on cold and flu, hot flashes and irritable bowel syndrome. In the Oregon study, 60 people received five hours of either relaxation training or Mindful Meditation training. Among the smokers in the study, there was no difference in the amount the relaxation group smoked. However, the smokers in the meditation group had cut back by 60 percent. Researchers admit that the smoking findings are surprising, and caution that the study was very small. Also, the participants were all college students. On the other hand, none of the subjects were told they were taking part in a smoking study. And the Oregon study found that the brains of the smokers who learned meditation techniques were more active in an area linked to self-control. More work in this area is warranted.
 Painkiller Overdoses Spiking Among Women A new report from the Centers for Disease Control offers some eye-opening facts on the abuse of painkillers among women. Since 1999, the number of women who have died from a painkiller overdose has increased by a factor of four. “Mothers, wives, sisters, and daughters are dying at rates that we have never seen before,” says Dr. Thomas Frieden, Director of the CDC. Among the more alarming aspects of the report are: 1) On average, 18 women die
Painkiller Overdoses Spiking Among Women A new report from the Centers for Disease Control offers some eye-opening facts on the abuse of painkillers among women. Since 1999, the number of women who have died from a painkiller overdose has increased by a factor of four. “Mothers, wives, sisters, and daughters are dying at rates that we have never seen before,” says Dr. Thomas Frieden, Director of the CDC. Among the more alarming aspects of the report are: 1) On average, 18 women die  from painkiller overdoses in the U.S. every day; 2) More women die from prescription drug overdoses than from car accidents; 3) Some 50,000 women between the ages of 25 and 34 will be taken to U.S. emergency rooms as a result of painkiller overdoses this year. In its report, the CDC recommended that healthcare providers exercise greater caution when prescribing prescription medications—and suggested that states and the federal government could turn this trend around by doing a better job educating women on the dangers of prescription painkillers. “We are seeing an increase in the numbers of women and young people presenting in the emergency room with prescription pain and anxiety medications—many of whom have legitimate prescriptions for a physical or mental health disorder, and others who are accessing prescription meds from others or on the street,” Lisa Dressner confirms. Dressner is Program Director of TRMC’s Psychiatric Emergency Services. “Too often, alternatives to these highly addictive medications are not explored, and primary care or pain management doctors may not fully assess someone’s potential or history of substance abuse.” There is an urgent need, she adds, for more education to consumers around the potential for addiction to commonly prescribed pain meds, and medications for problems related to anxiety or sleep, so that risk for abuse of these medications, and increased depression, withdrawal and suicidality is minimized.
from painkiller overdoses in the U.S. every day; 2) More women die from prescription drug overdoses than from car accidents; 3) Some 50,000 women between the ages of 25 and 34 will be taken to U.S. emergency rooms as a result of painkiller overdoses this year. In its report, the CDC recommended that healthcare providers exercise greater caution when prescribing prescription medications—and suggested that states and the federal government could turn this trend around by doing a better job educating women on the dangers of prescription painkillers. “We are seeing an increase in the numbers of women and young people presenting in the emergency room with prescription pain and anxiety medications—many of whom have legitimate prescriptions for a physical or mental health disorder, and others who are accessing prescription meds from others or on the street,” Lisa Dressner confirms. Dressner is Program Director of TRMC’s Psychiatric Emergency Services. “Too often, alternatives to these highly addictive medications are not explored, and primary care or pain management doctors may not fully assess someone’s potential or history of substance abuse.” There is an urgent need, she adds, for more education to consumers around the potential for addiction to commonly prescribed pain meds, and medications for problems related to anxiety or sleep, so that risk for abuse of these medications, and increased depression, withdrawal and suicidality is minimized. other developed countries. Only a third of American girls have been fully vaccinated; in other countries (including Rwanda!) the rate is closer to 80 percent. HPV causes 19,000 cases of cancer among women in the U.S. each year. It also accounts for 8,000 cases in men, a statistic brought to light by actor Michael Douglas, whose throat cancer was identified as being HPV-related. “The study showed that less than four years later the prevalence of the vaccine strains among young women aged 14–19 years had fallen by 56%,” points out Dr. William Farrer, Associate Program Director and Associate Professor of Medicine of the Seton Hall University School of Health and Medical Sciences at TRMC. “This was despite the fact that in 2010, only 32% of 13–17 year-olds had received the full 3-dose series of vaccine. Rates of HPV infection in older women had not fallen, probably reflecting the fact that they were not the target group for the vaccine.The researchers also reported that ‘Sexual behavior among females aged 14–19 years overall was similar in the two periods.’ This should reassure opponents of the HPV vaccine who expressed concern that somehow use of the vaccine would encourage promiscuity.”
other developed countries. Only a third of American girls have been fully vaccinated; in other countries (including Rwanda!) the rate is closer to 80 percent. HPV causes 19,000 cases of cancer among women in the U.S. each year. It also accounts for 8,000 cases in men, a statistic brought to light by actor Michael Douglas, whose throat cancer was identified as being HPV-related. “The study showed that less than four years later the prevalence of the vaccine strains among young women aged 14–19 years had fallen by 56%,” points out Dr. William Farrer, Associate Program Director and Associate Professor of Medicine of the Seton Hall University School of Health and Medical Sciences at TRMC. “This was despite the fact that in 2010, only 32% of 13–17 year-olds had received the full 3-dose series of vaccine. Rates of HPV infection in older women had not fallen, probably reflecting the fact that they were not the target group for the vaccine.The researchers also reported that ‘Sexual behavior among females aged 14–19 years overall was similar in the two periods.’ This should reassure opponents of the HPV vaccine who expressed concern that somehow use of the vaccine would encourage promiscuity.” Air Pollution Linked to Sleep Disorders in Children While we watch the Arab Spring unfold in Egypt in dramatic fashion, some dramatic health news has come out of that country that is relevant right here in New Jersey. In July, University of Cairo researchers announced the results of sleep study on school-age children, which shows a link between air pollution and sleep disorders. The 276 children in the study exhibited significant disorders of initiating and maintaining sleep, and excessive
Air Pollution Linked to Sleep Disorders in Children While we watch the Arab Spring unfold in Egypt in dramatic fashion, some dramatic health news has come out of that country that is relevant right here in New Jersey. In July, University of Cairo researchers announced the results of sleep study on school-age children, which shows a link between air pollution and sleep disorders. The 276 children in the study exhibited significant disorders of initiating and maintaining sleep, and excessive  somnolence when exposed to PM10 (particulate matter smaller than 10 micrometers) in the air. PM10 particles can settle in the lungs and cause health problems. Larger particles are typically filtered by the nose and throat. In treating the pediatric population at the Trinitas Comprehensive Sleep Disorders Center, Vipin Garg, MD, Director of the Center notes that, “Small particles or large particles of pollution can irritate the airways of children, especially those who have large adenoids. Children who have to breathe through their mouths because of enlarged adenoids bypass the normal filtering process of the nose and that can have an irritant effect on both the upper and lower airways. This may result in a significant sleep disturbance especially if sleep is already compromised. Also lower airway irritation can lead to asthma-like symptoms.”
somnolence when exposed to PM10 (particulate matter smaller than 10 micrometers) in the air. PM10 particles can settle in the lungs and cause health problems. Larger particles are typically filtered by the nose and throat. In treating the pediatric population at the Trinitas Comprehensive Sleep Disorders Center, Vipin Garg, MD, Director of the Center notes that, “Small particles or large particles of pollution can irritate the airways of children, especially those who have large adenoids. Children who have to breathe through their mouths because of enlarged adenoids bypass the normal filtering process of the nose and that can have an irritant effect on both the upper and lower airways. This may result in a significant sleep disturbance especially if sleep is already compromised. Also lower airway irritation can lead to asthma-like symptoms.” Walking the Walk While the medical profession has long promoted the benefits of daily exercise, a new study out of the Middle East pinpoints how short, brisk walks taken after meals are an effective way to diminish the risk of developing Type 2 diabetes. The results, published in the latest issue of Diabetes Care, focus on how post-meal strolls reduce blood sugar levels. “Blood sugar levels are the highest after meals and as we age our pancreas is less effective in releasing insulin, a hormone that helps lower blood sugar,”
Walking the Walk While the medical profession has long promoted the benefits of daily exercise, a new study out of the Middle East pinpoints how short, brisk walks taken after meals are an effective way to diminish the risk of developing Type 2 diabetes. The results, published in the latest issue of Diabetes Care, focus on how post-meal strolls reduce blood sugar levels. “Blood sugar levels are the highest after meals and as we age our pancreas is less effective in releasing insulin, a hormone that helps lower blood sugar,”  explains Dr. Mahmoud Ali Zirie, who ran the study out of Qatar. “This leads to higher blood sugar that can increase the risk of diabetes. A short walk two hours after meals can help normalize blood sugar levels. To achieve maximum health benefits walking should be moderate intensity. In other words, it needs to be faster than a stroll and brisk enough to raise your heart rate.” Those who are new to this type of exercise should begin slowly, stay hydrated and avoid excessive heat, and build toward a regular and rigorous regimen. Kathleen McCarthy, RN, a Certified Diabetes Educator at Trinitas, offers these tips: “Whether you have diabetes or you are trying to keep diabetes at arm’s length, you will benefit from a regular exercise regimen of 30 minutes a day, five days a week, or more. Short brisk walks, two hours after a meal, improve post-prandial (after meal) glucose readings. Walking also improves circulation, heart and lung function, and releases endorphins which help control of stress and pain. As you build muscle mass, your metabolism will increase which then gives you more energy and will lead to weight loss over time. The benefits of aerobic exercise last up to 12 hours after exercise. Exercise is a key ingredient to improve or maintain optimal health.”
explains Dr. Mahmoud Ali Zirie, who ran the study out of Qatar. “This leads to higher blood sugar that can increase the risk of diabetes. A short walk two hours after meals can help normalize blood sugar levels. To achieve maximum health benefits walking should be moderate intensity. In other words, it needs to be faster than a stroll and brisk enough to raise your heart rate.” Those who are new to this type of exercise should begin slowly, stay hydrated and avoid excessive heat, and build toward a regular and rigorous regimen. Kathleen McCarthy, RN, a Certified Diabetes Educator at Trinitas, offers these tips: “Whether you have diabetes or you are trying to keep diabetes at arm’s length, you will benefit from a regular exercise regimen of 30 minutes a day, five days a week, or more. Short brisk walks, two hours after a meal, improve post-prandial (after meal) glucose readings. Walking also improves circulation, heart and lung function, and releases endorphins which help control of stress and pain. As you build muscle mass, your metabolism will increase which then gives you more energy and will lead to weight loss over time. The benefits of aerobic exercise last up to 12 hours after exercise. Exercise is a key ingredient to improve or maintain optimal health.” Mild Depression and Alzheimer’s A recent aging study conducted by researchers in the U.S. and Asia has found that the onset of Alzheimer’s Disease appears to be accelerated by depression. The study suggested that individuals with depressive symptoms progressed from mild cognitive impairment to full-blown Alzheimer’s at a much faster rate than those who did not exhibit signs of depression. Indeed, depression doubled the risk of developing Alzheimer’s in this particular study. These findings have opened
Mild Depression and Alzheimer’s A recent aging study conducted by researchers in the U.S. and Asia has found that the onset of Alzheimer’s Disease appears to be accelerated by depression. The study suggested that individuals with depressive symptoms progressed from mild cognitive impairment to full-blown Alzheimer’s at a much faster rate than those who did not exhibit signs of depression. Indeed, depression doubled the risk of developing Alzheimer’s in this particular study. These findings have opened  up a number of debates about what actually triggers the cognitive decline. However, it strongly suggests that decisive steps to intervene or mediate depression among people at risk for Alzheimer’s need to be taken. “Occasionally, depression in the elderly, even in the absence of dementia, has been known to result in impairment of cognitive functions,” adds Dr. Anwar Y. Ghali, Chairman of Psychiatry at Trinitas. “Especially the memory, in a condition referred to as ‘depressive pseudo dementia.’ Hence, one would expect that this might occur at a higher rate with patients already diagnosed with Alzheimer’s. Therefore, physicians should always evaluate Alzheimer’s patients for the possibility of a co-morbid depression. With adequate treatment of depression, patients should be relieved of suffering and also experience reduced possibility of suicide—a complication of depression that occurs at a higher rate with the elderly, especially in males and particularly for those suffering from an additional illness.”
up a number of debates about what actually triggers the cognitive decline. However, it strongly suggests that decisive steps to intervene or mediate depression among people at risk for Alzheimer’s need to be taken. “Occasionally, depression in the elderly, even in the absence of dementia, has been known to result in impairment of cognitive functions,” adds Dr. Anwar Y. Ghali, Chairman of Psychiatry at Trinitas. “Especially the memory, in a condition referred to as ‘depressive pseudo dementia.’ Hence, one would expect that this might occur at a higher rate with patients already diagnosed with Alzheimer’s. Therefore, physicians should always evaluate Alzheimer’s patients for the possibility of a co-morbid depression. With adequate treatment of depression, patients should be relieved of suffering and also experience reduced possibility of suicide—a complication of depression that occurs at a higher rate with the elderly, especially in males and particularly for those suffering from an additional illness.” Landmark Diabetes Study Completed The recently completed Look AHEAD study by the University of Pittsburgh has brought into question the value of lifestyle intervention programs for overweight and obese Type 2 diabetes patients. The study covered more than 5,000 people at 16 clinical centers across the country, over more than a decade. One group in the study followed an aggressive program of weight management and increased physical activity. The other was only provided with health information and support related to diabetes. In terms of strokes and heart attacks, there was no significant difference between the two groups. The biggest difference between the groups was in the area of weight loss. The information and support group lost relatively little weight, while the intervention group lost 8.7 percent of their body weight and had excellent success keeping it off. A 5 percent weight loss is considered clinically significant, particularly in the controlling of cholesterol, blood pressure and blood sugar. “While the findings from the Look AHEAD study did not support that
Landmark Diabetes Study Completed The recently completed Look AHEAD study by the University of Pittsburgh has brought into question the value of lifestyle intervention programs for overweight and obese Type 2 diabetes patients. The study covered more than 5,000 people at 16 clinical centers across the country, over more than a decade. One group in the study followed an aggressive program of weight management and increased physical activity. The other was only provided with health information and support related to diabetes. In terms of strokes and heart attacks, there was no significant difference between the two groups. The biggest difference between the groups was in the area of weight loss. The information and support group lost relatively little weight, while the intervention group lost 8.7 percent of their body weight and had excellent success keeping it off. A 5 percent weight loss is considered clinically significant, particularly in the controlling of cholesterol, blood pressure and blood sugar. “While the findings from the Look AHEAD study did not support that  engagement in a weight-loss intervention was effective for reducing the onset of cardiovascular disease incidence or mortality, this does not mean that overweight adults with diabetes should not lose weight and become more physically active,” says John Jakicic of the Department of Health and Physical Activity in Pitt’s School of Education. Dr. Ari Eckman, Chief of Endocrinology and Metabolism at Trinitas, adds that there is an overwhelming amount of evidence from this study to date that has shown that weight loss and physical activity were associated with numerous other health benefits: “While weight loss alone was not shown to significantly decrease this incidence in the recent Look AHEAD study, there is strong support from numerous studies supporting the benefits of weight loss and physical activity for many other health benefits. Further studies are recommended to determine the full effect weight loss has on cardiovascular disease prevention. It is still strongly recommended for people with diabetes who are overweight or obese to lose weight and maintain a healthy lifestyle.”
engagement in a weight-loss intervention was effective for reducing the onset of cardiovascular disease incidence or mortality, this does not mean that overweight adults with diabetes should not lose weight and become more physically active,” says John Jakicic of the Department of Health and Physical Activity in Pitt’s School of Education. Dr. Ari Eckman, Chief of Endocrinology and Metabolism at Trinitas, adds that there is an overwhelming amount of evidence from this study to date that has shown that weight loss and physical activity were associated with numerous other health benefits: “While weight loss alone was not shown to significantly decrease this incidence in the recent Look AHEAD study, there is strong support from numerous studies supporting the benefits of weight loss and physical activity for many other health benefits. Further studies are recommended to determine the full effect weight loss has on cardiovascular disease prevention. It is still strongly recommended for people with diabetes who are overweight or obese to lose weight and maintain a healthy lifestyle.”