A pair of TRMC newcomers bring a healthy dose of hope.
By Christine Gibbs
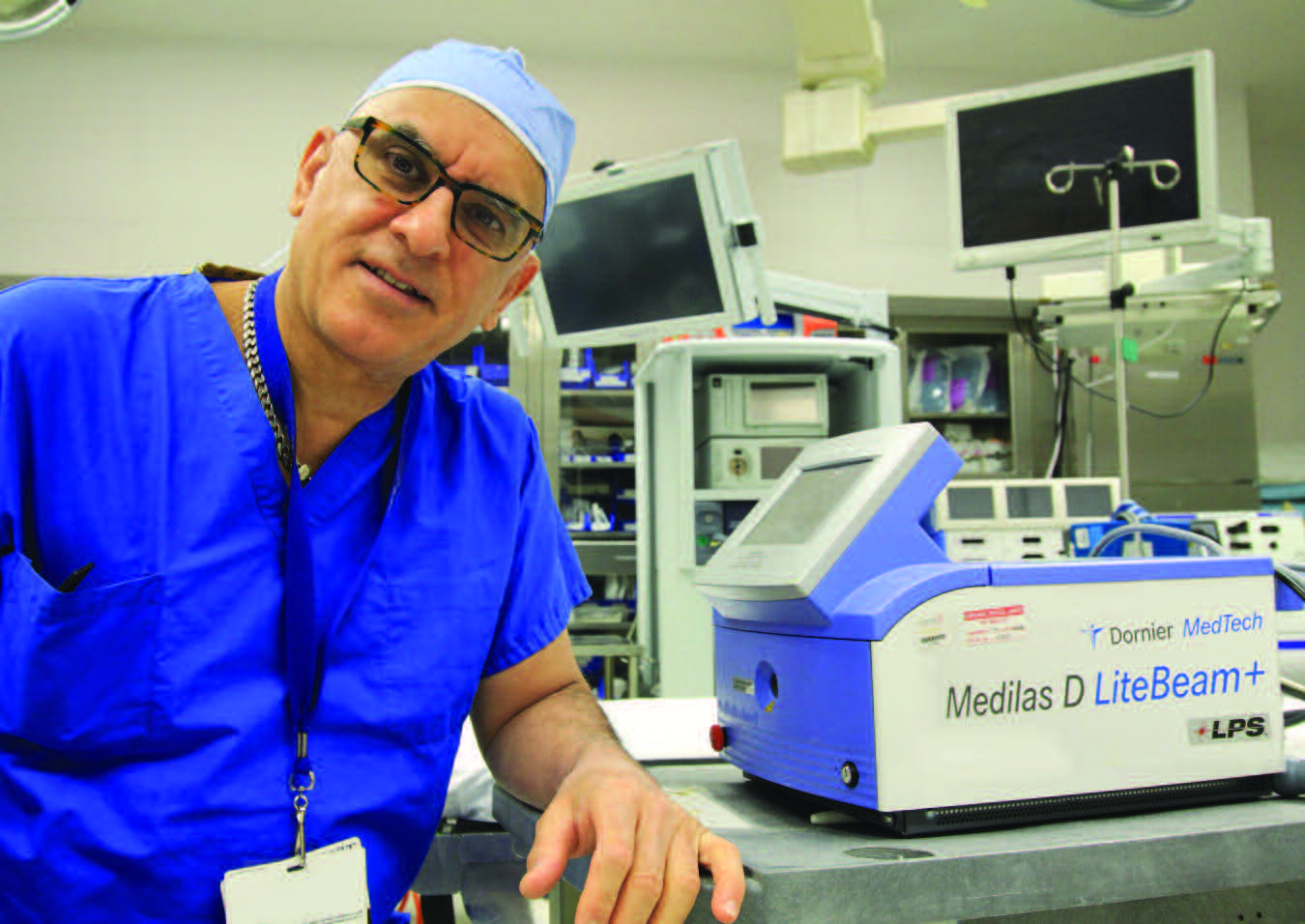
Not all that long ago, a diagnosis of liver or pancreatic disease would strike fear in the heart of a patient. Now there is hope on the horizon thanks to new treatment options, especially when an early diagnosis is involved. That hope is embodied in a pair of highly skilled surgeons that recently joined the Trinitas Regional Medical Center staff: Dr. Lloyd Brown and Dr. Baburao Koneru, both of whom are hepatopancreatobiliary (HPB) specialists.
Dr. Koneru, came aboard as an attending surgeon at TRMC in 2015, has been practicing his specialty for 39 years. Dr. Brown has been on staff in the Surgery Department since early 2016. Both doctors are part of the Division of Liver Transplant and Hepatobiliary Surgery at University Hospital. In addition to their intense surgical responsibilities, they find time to share their expertise as professors at the Rutgers Medical School, in Newark. “The liver is the only organ that can regenerate itself, which is why live donors are acceptable for transplanting,” says Dr. Brown (left), who specializes in liver transplants and resections. “Only 30 percent of the liver is absolutely necessary to survive, making it possible to safely remove two-thirds of the liver of a living donor. And it takes only a few months for 75 to 80 percent of the organ to regenerate itself.”

Dr. Koneru (right) focuses on surgical treatments of
both the liver and the pancreas. One of the procedures he uses on certain of his pancreatic cancer patients is the Whipple resection, where portions of the pancreas can be safely removed. When treating liver diseases, Dr. Koneru says that ablation as a technique is frequently recommended. Ablation involves surgical destruction of diseased tissue through a variety of procedures, including chemical ablations, microwave ablations (which employ heat energy), and radiofrequency ablations (which use high-energy radio waves to destroy cancerous cells).

Dr. Brown and Dr. Koneru were drawn to HPB surgical careers for similar reasons.
“I have always had an interest in pursuing a profession requiring a high degree of medical skills that would help patients through a personal crisis in their life,” says Dr. Brown. “I believe that surgery is a fascinating life-long learning experience.”
Dr. Koneru says that he too became fascinated with the opportunity to “manage treatment of highly complex disorders that require detailed patient information analysis and highly developed skills.” He also emphasized his commitment to “the challenge of providing the best post-surgical patient care possible.”
Despite a relatively brief time at Trinitas, both doctors have positive things to say about the experience. Dr. Brown describes the environment in the Surgical Department as very collegial, with excellent channels of communication—which is critical to optimizing each surgeon’s performance. Dr. Koneru praises the efficiency of the operating room and intensive care units, as well as the quality of care provided by the regular nursing staff. He describes Trinitas as “simultaneously patient- and physician-friendly.” Dr. Koneru also appreciates the opportunity to provide expert care to patients in the greater Elizabeth area.
As for the future of HPB surgery, the greatest strides, they agree, will be made in minimally invasive robotic-assisted surgery. “We have already begun to develop the minimally invasive and robotic-assisted Hepatobiliary surgery practice here at Trinitas,” points out Dr. Brown, who recently performed three robotic-assisted cases. He is convinced that Trinitas will continue its policy of acquiring the best and latest equipment—which will result in increased positive outcomes—and that Trinitas surgeons will continue to pursue the latest advances in surgical techniques. Dr. Koneru adds that, in addition to robotic techniques being used more widely, the number of surgeons with cutting-edge expertise in the field will increase: “That will make more of them available to join the staff of many smaller hospitals, which can then provide higher quality treatment locally.”
Both doctors envision the success rates for HPB patient surgeries to continue to improve.
 HEP C
HEP C
Today Hepatitis C, one of the viral infections that causes liver inflammation, has been receiving much media attention. Although there are five types of hepatitis—from A through E—it is Hep C that is having the greatest impact on the Boomer population. Statistics indicate that 1 in 30 Boomers is infected with Hep C, but not all of those infected know it. If left untreated, the disease can cause potentially fatal liver complications.
A simple blood test during your next doctor appointment can determine whether you have Hepatitis C. If the result is positive, all you may need is a script for ribavirin, a drug recently approved by the FDA, which interrupts the virus’s ability to replicate. Clinical tests have shown a 98 percent cure rate—more than double that of the drugs it replaces.
 Lloyd Brown, MD, MS
Lloyd Brown, MD, MS
HPB Specialist
Assistant Professor of Surgery Division of Liver Transplant & Hepatobiliary Surgery
Rutgers New Jersey Medical School 973.972.2408
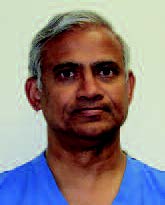 Baburao Koneru, MD, MPH HPB Specialist
Baburao Koneru, MD, MPH HPB Specialist
Professor of Surgery
Division of Liver Transplant & Hepatobiliary Surgery
Rutgers New Jersey Medical School 973.972.2408


 The Hidden Costs of Strokes
The Hidden Costs of Strokes 
 Postpartum Issues Beyond Depression
Postpartum Issues Beyond Depression 
 Could Obesity be a Mental Illness?
Could Obesity be a Mental Illness? Working Out Heart Attack Symptoms
Working Out Heart Attack Symptoms 
 Does Natural Selection Still
Does Natural Selection Still  Low-Dose Recommendation
Low-Dose Recommendation 

 Geriatric patients will be seen in a separate, more serene area—with cosmetic and practical improvements and additions, such as mobility aids, pressure-reducing mattresses, bedside commodes, bedside transition stools, and the use of non-slip socks and hearing aids. Even the clocks on the walls are larger. But not only seniors will benefit from improvements and the 18 additional beds—including five private Geriatric beds, six Transitional Care Unit beds, and seven Fast Track Treatment bays. According to Dr. John D’Angelo, Chairman of the Emergency Medicine Department, the Geriatric ED has more to do with the complexity of care and less to do with age.
Geriatric patients will be seen in a separate, more serene area—with cosmetic and practical improvements and additions, such as mobility aids, pressure-reducing mattresses, bedside commodes, bedside transition stools, and the use of non-slip socks and hearing aids. Even the clocks on the walls are larger. But not only seniors will benefit from improvements and the 18 additional beds—including five private Geriatric beds, six Transitional Care Unit beds, and seven Fast Track Treatment bays. According to Dr. John D’Angelo, Chairman of the Emergency Medicine Department, the Geriatric ED has more to do with the complexity of care and less to do with age.  However, Dr. D’Angelo—who also serves as a tactical physician for the Union County Emergency Response Team and the SWAT Team—says, “Preparing for the unexpected is always a challenge. Patient arrivals on any given day at any given hour can be very dynamic. We are determined to answer the call through thoughtful staffing patterns and continued process improvement.”
However, Dr. D’Angelo—who also serves as a tactical physician for the Union County Emergency Response Team and the SWAT Team—says, “Preparing for the unexpected is always a challenge. Patient arrivals on any given day at any given hour can be very dynamic. We are determined to answer the call through thoughtful staffing patterns and continued process improvement.”
 “Part of it is to see yourself within your patients,” he explains. “I see you; I am you. That’s critical in the delivery of the healthcare delivery system—to see yourself in the individual who is struggling.”
“Part of it is to see yourself within your patients,” he explains. “I see you; I am you. That’s critical in the delivery of the healthcare delivery system—to see yourself in the individual who is struggling.” 
 “Our recovery specialist encountered the patient when he was sober,” Dr. D’Angelo recalls. “They made arrangements to meet at a McDonald’s for a free breakfast and coffee. The patient’s only obligation was sobriety.”
“Our recovery specialist encountered the patient when he was sober,” Dr. D’Angelo recalls. “They made arrangements to meet at a McDonald’s for a free breakfast and coffee. The patient’s only obligation was sobriety.”

 Four Months or Twelve?
Four Months or Twelve?  Home Care of Alzheimer’s Patients On the Rise
Home Care of Alzheimer’s Patients On the Rise  Is Vaping Worse for You Than Smoking?
Is Vaping Worse for You Than Smoking?  Easy On the Knees
Easy On the Knees  Pedaling Toward Happiness
Pedaling Toward Happiness 

 TAKING NOTHING FOR GRANTED
TAKING NOTHING FOR GRANTED
 Indeed, Dr. Cordero is proud of the fact that he has performed more than 800 carotid endarterectomy surgeries, with very few complications and zero deaths. In addition to a high success rate, it’s worth noting that his is a solo practice in a corner of the world where group practices are more common.
Indeed, Dr. Cordero is proud of the fact that he has performed more than 800 carotid endarterectomy surgeries, with very few complications and zero deaths. In addition to a high success rate, it’s worth noting that his is a solo practice in a corner of the world where group practices are more common.
 “Eating healthy is one of those things I’ve been meaning to do, but had a hard time with,” says Rumola, a 36-year-old stay-at-home mom whose children are 13 and 10. “The Mobile Market is such a help because we get fresh vegetables and fruits, which means a few less dollars I have to spend. But they also give us recipes…and I’ve learned about portions, saturated fat, and things I didn’t know before.”
“Eating healthy is one of those things I’ve been meaning to do, but had a hard time with,” says Rumola, a 36-year-old stay-at-home mom whose children are 13 and 10. “The Mobile Market is such a help because we get fresh vegetables and fruits, which means a few less dollars I have to spend. But they also give us recipes…and I’ve learned about portions, saturated fat, and things I didn’t know before.”

 Crunch Time
Crunch Time 
 Into the Woods
Into the Woods  Cervical Cancer’s “Racial Divide”
Cervical Cancer’s “Racial Divide”  But Is It An Organ?
But Is It An Organ?  Real-Time Concussion Detector
Real-Time Concussion Detector 
 Early Detection for Autism
Early Detection for Autism 

 Seven are high-fidelity computer-operated mannequins that have heartbeats, can breathe, talk, sweat and simulate a wide range of medical conditions and responses to treatment. Two are birthing simulators that can simulate the birth of a baby and the complications of pregnancy and childbirth. Also featured in the lab are part-task simulation trainers. These are smaller simulation pieces of equipment that mimic specific parts of the human body. They are used to practice delicate procedures, such as intravenous therapy, urinary catheterization and colostomy care.
Seven are high-fidelity computer-operated mannequins that have heartbeats, can breathe, talk, sweat and simulate a wide range of medical conditions and responses to treatment. Two are birthing simulators that can simulate the birth of a baby and the complications of pregnancy and childbirth. Also featured in the lab are part-task simulation trainers. These are smaller simulation pieces of equipment that mimic specific parts of the human body. They are used to practice delicate procedures, such as intravenous therapy, urinary catheterization and colostomy care.  The Learning/Simulation Center also includes a digital audio-visual system that transmits and records situations in a simulated environment to facilitate learning. Control rooms for the simulation area permit instructors and computer specialists to remotely operate the mannequins. An adjacent debriefing room enables instructors and students to review the video recording of the simulated scenario and engage in a reflective discussion of what occurred during that simulation. The Learning/Simulation Center is just one more example of how TSON continues to enhance students’ learning environment and promote professional growth.
The Learning/Simulation Center also includes a digital audio-visual system that transmits and records situations in a simulated environment to facilitate learning. Control rooms for the simulation area permit instructors and computer specialists to remotely operate the mannequins. An adjacent debriefing room enables instructors and students to review the video recording of the simulated scenario and engage in a reflective discussion of what occurred during that simulation. The Learning/Simulation Center is just one more example of how TSON continues to enhance students’ learning environment and promote professional growth. 


 Mobin Chadha, LCSW
Mobin Chadha, LCSW 
 Seventeen years ago, President Bill Clinton officially set aside March as National Colon Cancer Awareness Month. On the 3rd of the month this year, you’ll see a lot of blue stars around; that Friday is Dress in Blue Day (dressinblueday.org). The good news is that, since 2000, there has been a marked drop in colorectal cancer incidence—more than 30 percent among Americans 50 and older. The distressing news is that,
Seventeen years ago, President Bill Clinton officially set aside March as National Colon Cancer Awareness Month. On the 3rd of the month this year, you’ll see a lot of blue stars around; that Friday is Dress in Blue Day (dressinblueday.org). The good news is that, since 2000, there has been a marked drop in colorectal cancer incidence—more than 30 percent among Americans 50 and older. The distressing news is that, 

 Facebook took a lot of heat for propagating “fake news” during the past election, but according to researchers at Lancaster University, there’s something even more depressing: Facebook itself. In a survey of 35,000 people between the ages of 15 and 88, the Lancaster study found that Facebook users who compared themselves negatively with others were at increased risk of depression. Those at greatest risk were individuals who “friended” former partners, made frequent negative status updates or felt intense envy when they observed the “life highlights” of others. The research did point out that social media engagement could also help with depression—when used as a mental health resource or to enhance social support.
Facebook took a lot of heat for propagating “fake news” during the past election, but according to researchers at Lancaster University, there’s something even more depressing: Facebook itself. In a survey of 35,000 people between the ages of 15 and 88, the Lancaster study found that Facebook users who compared themselves negatively with others were at increased risk of depression. Those at greatest risk were individuals who “friended” former partners, made frequent negative status updates or felt intense envy when they observed the “life highlights” of others. The research did point out that social media engagement could also help with depression—when used as a mental health resource or to enhance social support. 
 More and more women are becoming mothers in their late 30s and 40s than ever before. Although there are certain health risks associated with later pregnancies, researchers at the University of Southern California report that women who have their final baby at age 35 or older appear to have an advantage later in life. The USC study looked at 830 post-menopausal women and noticed that those who had their last baby at age 35 or older had sharper cognitive skills at age 60 than women who stopped bearing children earlier on. Dr. Roksana Karim, who led the study, noted that she would not advise women to wait and have their final child after age 35.
More and more women are becoming mothers in their late 30s and 40s than ever before. Although there are certain health risks associated with later pregnancies, researchers at the University of Southern California report that women who have their final baby at age 35 or older appear to have an advantage later in life. The USC study looked at 830 post-menopausal women and noticed that those who had their last baby at age 35 or older had sharper cognitive skills at age 60 than women who stopped bearing children earlier on. Dr. Roksana Karim, who led the study, noted that she would not advise women to wait and have their final child after age 35. While medical researchers brave the wilds of the Amazon and other remote regions of the world to look for new medicines, researchers from Rockefeller University have discovered promising microbes a bit closer to home: in the dirt of New York City parks. According to the Proceedings of the National Academy of Sciences, researchers tested 275 samples and found genetic evidence of bacteria capable of producing a wide array of compounds that can be harnessed for new medicines for cancer, as well as for bacterial and fungal infections. “The sheer diversity we saw suggests there are many more potentially valuable compounds out there awaiting discovery,” says Professor Sean Brady, who heads up Rockefeller’s Laboratory of Genetically Encoded Small Molecules. “Even in a place as mundane as urban soil.” One sample from Brooklyn contained genes that encode 25 molecules that are being studied for potential use as antibiotics and other types of medicines.
While medical researchers brave the wilds of the Amazon and other remote regions of the world to look for new medicines, researchers from Rockefeller University have discovered promising microbes a bit closer to home: in the dirt of New York City parks. According to the Proceedings of the National Academy of Sciences, researchers tested 275 samples and found genetic evidence of bacteria capable of producing a wide array of compounds that can be harnessed for new medicines for cancer, as well as for bacterial and fungal infections. “The sheer diversity we saw suggests there are many more potentially valuable compounds out there awaiting discovery,” says Professor Sean Brady, who heads up Rockefeller’s Laboratory of Genetically Encoded Small Molecules. “Even in a place as mundane as urban soil.” One sample from Brooklyn contained genes that encode 25 molecules that are being studied for potential use as antibiotics and other types of medicines. So your big New Year’s resolution was to try your first 5K run this spring? Where there’s a will, there’s a way as they say. But you may need to do more than buy a
So your big New Year’s resolution was to try your first 5K run this spring? Where there’s a will, there’s a way as they say. But you may need to do more than buy a
 The future of healthcare is a topic of considerable debate in this country. Experts will argue endlessly the pros, cons and particulars of the various industry sectors, and consumer advocates will probably be battling with insurance companies until the end of time. Interestingly, there is one thing everyone seems to agree on: Integration of services is the key to any real
The future of healthcare is a topic of considerable debate in this country. Experts will argue endlessly the pros, cons and particulars of the various industry sectors, and consumer advocates will probably be battling with insurance companies until the end of time. Interestingly, there is one thing everyone seems to agree on: Integration of services is the key to any real  Regional Medical Center and St. Joseph’s Regional Medical Center in Paterson forged an Integrated Behavioral Health Network—one of the largest and most comprehensive in the region. The partnership was announced in late 2016.
Regional Medical Center and St. Joseph’s Regional Medical Center in Paterson forged an Integrated Behavioral Health Network—one of the largest and most comprehensive in the region. The partnership was announced in late 2016. 


 The Trinitas-St. Joseph’s Behavioral Health Network brings together more than 700 employees and staff members with an annual budget of $50 million. Patients will have access to more than 40 psychiatrists. The Network will provide more than 350,000 outpatient contacts in 2017 and over 3,000 inpatient admissions.
The Trinitas-St. Joseph’s Behavioral Health Network brings together more than 700 employees and staff members with an annual budget of $50 million. Patients will have access to more than 40 psychiatrists. The Network will provide more than 350,000 outpatient contacts in 2017 and over 3,000 inpatient admissions.  DID YOU KNOW?
DID YOU KNOW?
 For some families, a spring vacation can “go South“ at the end of the jet way. Follow these three rules and at least you’ll get to your destination unscathed.
For some families, a spring vacation can “go South“ at the end of the jet way. Follow these three rules and at least you’ll get to your destination unscathed. According to Travel Channel, these warm-weather destinations are among the hottest family vacation targets for Spring ’17:
According to Travel Channel, these warm-weather destinations are among the hottest family vacation targets for Spring ’17: Yelena Samofalov, MD Trinitas Pediatric Health Center 908.994.5750
Yelena Samofalov, MD Trinitas Pediatric Health Center 908.994.5750
 You can quibble with these numbers—they rise and fall depending on clinical criteria and also who’s doing the studies—but there is no arguing that depression has a crippling effect on almost every aspect of the pursuit of happiness in America. On one end of the spectrum, it may involve temporary sadness (aka “the blues”). On the other end, it can last indefinitely, profoundly diminishing quality of life to the point of complete dysfunction. According to the Anxiety and Depression Association of America, depression is the leading cause of disability worldwide. People with depression may also suffer from anxiety disorders, which are different, but share similar symptoms—including insomnia, the inability to concentrate, nervousness, and irritability.
You can quibble with these numbers—they rise and fall depending on clinical criteria and also who’s doing the studies—but there is no arguing that depression has a crippling effect on almost every aspect of the pursuit of happiness in America. On one end of the spectrum, it may involve temporary sadness (aka “the blues”). On the other end, it can last indefinitely, profoundly diminishing quality of life to the point of complete dysfunction. According to the Anxiety and Depression Association of America, depression is the leading cause of disability worldwide. People with depression may also suffer from anxiety disorders, which are different, but share similar symptoms—including insomnia, the inability to concentrate, nervousness, and irritability.  The good news is that doctors have an ever-growing arsenal of pharmaceutical solutions. These medications have changed the game for millions of sufferers. The not so- good news is that a high percentage of individuals—as many as half of the 15 million people experiencing depression—either cannot tolerate or do not respond to these drugs.
The good news is that doctors have an ever-growing arsenal of pharmaceutical solutions. These medications have changed the game for millions of sufferers. The not so- good news is that a high percentage of individuals—as many as half of the 15 million people experiencing depression—either cannot tolerate or do not respond to these drugs. Elizabeth-based Medical Center assumes ownership of Bayonne Community Mental Health Center The healthcare world is in a rapid state of transformation where new opportunities often arise to elevate the level of care. Such an opportunity presented itself in 2017, when the Board of Trustees of Bayonne Community Mental Health Center (CMHC) elected to have Trinitas Regional Medical Center assume ownership of the CMHC. “This transition to ownership by Trinitas promises to be as seamless as possible. There are no plans for any interruption or major changes in the name, services, personnel, hours, location or anything else that would impact the clientele or the community,” explained Joseph M. Kadian, Psy.D., President and CEO of the CMHC.
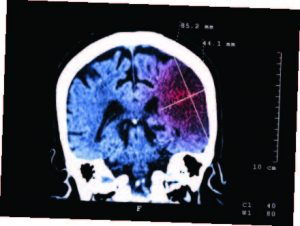
Elizabeth-based Medical Center assumes ownership of Bayonne Community Mental Health Center The healthcare world is in a rapid state of transformation where new opportunities often arise to elevate the level of care. Such an opportunity presented itself in 2017, when the Board of Trustees of Bayonne Community Mental Health Center (CMHC) elected to have Trinitas Regional Medical Center assume ownership of the CMHC. “This transition to ownership by Trinitas promises to be as seamless as possible. There are no plans for any interruption or major changes in the name, services, personnel, hours, location or anything else that would impact the clientele or the community,” explained Joseph M. Kadian, Psy.D., President and CEO of the CMHC. 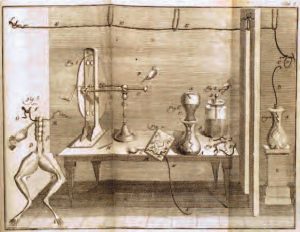 The field of Electrophysiology (of which Transcranial Magnetic Stimulation is a part) is nothing new. In fact, it dates back centuries. Near the end of the 18th century, Luigi Galvani first performed the same experiment you probably did in high-school Biology: noting that the legs of a dead frog twitched when touch by an electrical current. Galvani’s name is still with us today (galvanization). Several decades later, another giant in the history of science, Michael Faraday, did groundbreaking work in electromagnetism and electrochemistry, which established the foundation for research on brain stimulation through electricity and magnetism. By the mid-1900s, electroconvulsive therapy was widely used to treat major depression and other forms of mental illness. The first use of magnetic fields on electric signaling in the brain began in the 1980s, primarily for diagnostic purposes. By the early 2000s, however, researchers started noting the therapeutic possibilities of TMS.
The field of Electrophysiology (of which Transcranial Magnetic Stimulation is a part) is nothing new. In fact, it dates back centuries. Near the end of the 18th century, Luigi Galvani first performed the same experiment you probably did in high-school Biology: noting that the legs of a dead frog twitched when touch by an electrical current. Galvani’s name is still with us today (galvanization). Several decades later, another giant in the history of science, Michael Faraday, did groundbreaking work in electromagnetism and electrochemistry, which established the foundation for research on brain stimulation through electricity and magnetism. By the mid-1900s, electroconvulsive therapy was widely used to treat major depression and other forms of mental illness. The first use of magnetic fields on electric signaling in the brain began in the 1980s, primarily for diagnostic purposes. By the early 2000s, however, researchers started noting the therapeutic possibilities of TMS.
 A New Line in the Sand
A New Line in the Sand  Danger Alert for TV Binge Watchers
Danger Alert for TV Binge Watchers  Now Hear This
Now Hear This  Is Chocolate a “SAD” Solution?
Is Chocolate a “SAD” Solution?  Double Trouble
Double Trouble  Is That Cigarette Really Worth Seven Years?
Is That Cigarette Really Worth Seven Years?