My unlikely encounter with a silent epidemic.
By Dree Andrea
Twenty-five years had passed since my last visit to a doctor’s office. Which is why, in 2016, finding myself in a constant state of fear and paranoia, the thought of doing so never even crossed my mind. It happened practically overnight. I grew increasingly afraid of leaving my house. My dreams were so vivid that I started to confuse nightmares with reality. In order to (literally) save the day, my subconscious ordered the insomnia that followed. After five days without sleep, however, I became terrified of my fellow human beings. I had always considered myself a grounded, healthy, joyous person who met all the responsibilities that come with living life. I did my best to remain calm and logical, but I was also aware that my emotions were on the verge of total collapse, and would get the better of me sooner rather than later.
 A traumatic experience with the medical community early on in my life in Amsterdam (where I was born and raised) had motivated me to study a variety of holistic healing modalities after I came to America. When health issues arose that I could not address myself, I had worked successfully with a chiropractor and an acupuncturist, but never a traditional GP. Once, while experiencing severe pain after being clipped by a hit-and-run driver, a colleague convinced me to take an aspirin. It made me so sick that I decided to never touch over-the-counter medication again. Arnica gel for sprained ankles and Old Indian Wild Cherry bark for severe coughs were as far as I would go, no matter how grave the situation. I was a happy, healthy artist and documentary filmmaker living in the States for over 20 years when I began to “lose my mind.”
A traumatic experience with the medical community early on in my life in Amsterdam (where I was born and raised) had motivated me to study a variety of holistic healing modalities after I came to America. When health issues arose that I could not address myself, I had worked successfully with a chiropractor and an acupuncturist, but never a traditional GP. Once, while experiencing severe pain after being clipped by a hit-and-run driver, a colleague convinced me to take an aspirin. It made me so sick that I decided to never touch over-the-counter medication again. Arnica gel for sprained ankles and Old Indian Wild Cherry bark for severe coughs were as far as I would go, no matter how grave the situation. I was a happy, healthy artist and documentary filmmaker living in the States for over 20 years when I began to “lose my mind.”
Of course, my American friends had long questioned my sanity, albeit jokingly.

www.istockphoto.com
My belief that diet is the key to physical, emotional and mental health has made me an object of curiosity. On occasion, I have been called stubborn or even stupid for living my holistic lifestyle. I ate solely organic food and avoided sugar, coffee, and alcohol. I also exercised and practiced yoga and mindfulness. I learned through my own success—and as a graduate of the Natural Gourmet Institute in New York—that staying healthy (and doctor-free) takes a lot of time and attention, willpower and discipline. Eventually, I started coaching others—acquainting each client with the tools and techniques necessary to discover the lifestyle that worked best. In some cases, I imparted knowledge I had acquired in other areas, like Reiki, a form of hands-on healing developed in Japan. I also believed the key to balance and happiness was connecting to your creative self, whether through journaling, painting, cooking, or some other passion. I held art and cooking classes, as well as dream workshops. I was a Jack-of-all-trades with a stack of certificates, but no conventional degree. Even so, as the years went by, with a track record of positive reactions and referrals, I was satisfied that my degree in Life Experience was an acceptable alternative.
On paper, I was the last person who should have been swept away by this tsunami of negative energy. Over the previous seven years, I had dealt successfully with a series of unexpected stressful events, including a separation, the passing of a few dear friends, and working with a psychotic life-coaching client who turned out to be far more dangerous than I had been willing to admit while working with him. Also, I had recently made a major quality-of-life decision that I considered to be very positive. After two decades in a New York rental apartment, I had initiated a project that opened up the opportunity to purchase a fairytale weekend home in New Jersey, the perfect place to one day create a coaching practice and writer’s den. I knew the city eventually would become too demanding for the sensitive soul that—at age 50—I recognize that I am.
Most of my life I had been told to “not be so sensitive” and to “get over myself.” In 2010, however, I learned from one of the professionals with whom I worked that I am indeed an unusually (physically and emotionally) sensitive individual. Which is to say that I need a little less stimulus and a little more nature than the average person. So the location of the house—in a national historic district, with unpaved roads winding up and around a hillside overlooking the ocean, an absence of streetlights, friendly neighbors and lots of wildlife—was a dream come true. As technology has rushed forward, time has barely moved there. I saw it as a new phase in life. I hoped to find the community I missed in New York and I intended to practice what I preached, in order to eventually obtain my “Master’s” in Life Experience. Even if the unsettling experience with the aforementioned coaching client had taken place in this house, when my emotions started to unravel, I still felt peaceful there, protected by nature, thankful for this safe haven.
One day in November 2016, I entered my home and something seemed terribly wrong. Panic struck me like a bolt of lightning. I ran outside, finding myself standing under a full moon, in freezing weather, without a coat. The chill I felt was not from the cold. The house was haunted. The hill was haunted. “You’re going crazy,” I said out loud, trying to compose myself. “No one knows about it yet. And you better make sure they don’t find out!” Hearing my own words grounded me. I would rather die than get locked away in a psych ward. Thinking of the birds, crickets and squirrels with whom I cohabitate in this magical place, I took off my shoes and connected with Mother Earth. I had trained with shamans in Peru a decade earlier; Patcha Mama would come to my rescue, I just knew it. I had never felt so grateful in my life. “I’m no lunatic,” I declared, looking up to the huge, bright full moon.

www.istockphoto.com
However, in the ensuing months, I grew more and more tired. I started to lose my ability to concentrate or focus. I had completely lost my grip. I reacted to everything like a deer in the headlights. My self-confidence crumbled. It was like living outside of a box made of unbreakable, soundproof, see-through glass looking in, but at the same time being locked up inside that very same box, reaching out to myself for help. Neither of us could find a door to even knock on. I was a documentary filmmaker trapped in a horror movie.
Deep down inside, I sensed that I had just lost my way. I never lost my identity. Yet it was hard to continue to believe in myself as more and more people who had known me for a long time, when confronted with my personality change, seemed to be looking to create a little distance. I kept hearing that I appeared pretty healthy and, therefore, it could not really be that bad. Some suggested antidepressants, others that I get a dog. In my world, those were not solutions. I just wanted people to be part of my life again; I was desperately looking for support from humans, not animals. A caring neighbor who had attended and appreciated my dream workshops—and who was familiar with my diet— offered up another idea. She is all about finding balance, but seeks it in different places, in different ways than I do.

Dree AndreaShe suggested I might have a vitamin deficiency. The one thing I had not considered or tested were the levels of my vitamins, minerals, and hormones.
So it came to pass that I found myself in an examination room for the first time since the early 1990s. I was terrified of how an M.D. might approach whatever the outcome of the lab work would be but fortunately managed to find a doctor who was open to holistic modalities. It turned out that I did indeed have severe vitamin deficiencies—caused by long-term stress, which had taken its toll on both my sleep as well as my digestive system. Due to malabsorption, she said, I was dangerously low in B-12.
Dree Andrea
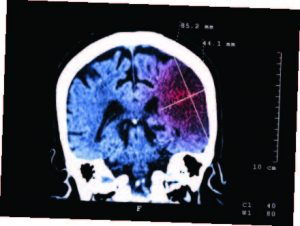
It turns out B-12 is a really big deal. It is one of the essential vitamins affecting various systems of the body. Neurologic, hematologic, gastrointestinal, as well as psychiatric symptoms, arise in cases of deficiency. The reason? Neurotransmitters communicate information throughout the brain and body, relaying signals between neurons. The brain uses neurotransmitters to let your heart know to keep beating, your lungs to inhale and exhale, and your stomach to digest. A lack of B-12 can also affect mood, sleep, concentration, and weight. Vitamin B-12 helps increase brain serotonin and dopamine levels because it is a cofactor in the synthesis of these neurotransmitters, as well as in norepinephrine and gamma-Aminobutyric acid (aka GABA)—the chief inhibitory neurotransmitter in the central nervous system. In humans, GABA also regulates muscle tone.
As I read up on B-12 deficiency, it was like reading my own story: Although not common, psychiatric symptoms may precede the physical ones, including fatigue, forgetfulness, loss of muscle strength, a feeling of pins-and-needles and change in vision. And wouldn’t you know it? The agitation, irritability, negativism, confusion, disorientation, amnesia, impaired concentration and attention and insomnia that a B-12 deficiency can also cause is often misdiagnosed as depression, bipolar or panic disorder, psychosis, phobias, or even dementia.
My doctor administered my first B-12 shot that very day. She warned me that it would take quite some time to start feeling better—up to six months. Me being me, I rushed home to do more research and discovered an alarming number of stories about people who had taken years to recover. A few had to get B- 12 shots for the rest of their lives.
As of December 2017, I had completed my fourth month of replenishing. From onset to diagnosis, almost a year had passed. I am glad to know that I am not going out of my mind.
During those months of self-doubt and uncertainty, a friend convinced me, quite forcefully, to see a therapist who, in turn, referred me to a trauma therapist. Those sessions actually left me questioning whether I would rise out of the ashes ever again. Therapy is not for everyone, and I sensed that this, at least for me, was not the right path. I continued exploring other options to find answers. Looking back, what now seems “crazy” to me is that going down the therapy path might very likely have resulted in a prescription for mood-altering psychotropic medication before my levels of vitamins, minerals, and hormones had been checked out first
And it is dawning on me that B-12 deficiency may be a silent epidemic. According to some studies, four in ten Americans, for example, are not getting enough B-12, while 60 percent of vegetarians and 90 percent (!) of vegans apparently are deficient. A growing number of medical professionals and therapists have also begun talking about a vulnerable third “high-risk” group: highly sensitive people, to which I belong. We perceive emotions, thoughts, and moods, energies, in such an intense way that we are often physically affected or even depleted by other people or situations, or by stimuli such as lights, sounds, or wifi radiation. In my case, adding a B-12 deficiency to an often confusing energy mix could have led to my personal short-circuit. Honestly, I felt I was blowing an emotional fuse. Had I wavered from the belief that I was not mentally ill, I could easily have ended up misdiagnosed with a mental disorder, on lithium or some other antidepressant.
In fact, I looped back to my physician after noticing my mood sink a few days after each B-12 injection—and then rise again while taking the sublingual (under-the tongue) B-12 in between shots. After a little more research, a new gameplan was formulated with the help of an orthomolecular practitioner, which involved no injections and a combination of two different types of sublingual B-12, 3000 mcg methylcobalamine and 3000 mcg adenosylcobalamine. Each one includes folic acid and is held under the tongue for a half-hour for optimal absorption.
Long story short, B-12 deficiency can be a complicated and highly personal journey. And because it is not part of the standard ordered lab work, it requires asking your doctor to test for B-12 if you suspect you have symptoms.
While my viewpoints on health and wellness have not significantly changed, I understand that the mind-body connection is not for everyone. I remain firm in my belief that physical problems arise as a result of something emotionally off-balance in life. During this whole ordeal, I knew that the path back to my old joyous and energetic self would require continuous truthful self-exploration, a combination of the right foods and supplements, and most of all patience. I am still not a huge fan of doctors, but I do recognize the value of a second opinion.
READ THE LABEL

www.istockphoto.com
My blood work revealed a number of vitamin and mineral deficiencies, for which I took various supplements to replenish. It was suggested that I try melatonin to help me sleep. That first night I woke up more often, feeling more severe disorientation and terror than ever before, so I immediately stopped taking it. A few weeks prior to this writing, I suddenly recalled that in my shamanic education we were told to take melatonin in combination with B-6 to enhance practicing lucid dreaming and astral travel. I myself had chosen not to take the supplements at the time. I decided to check the label on the bottle I bought a year ago. Sure enough, on the front in huge letters it said MELATONIN, but in examining the small print I found that the capsules contained a whopping 10 mg of B-6—500% of the daily recommended value!—in addition to the 1 mg of melatonin in each pill. I was shocked to find, returning to the health food store, what other ingredients are added to many vitamin supplements without a clear indication. Turns out we have to start reading those labels as carefully as we read the ones on our food.
 HUNTER GATHERER
HUNTER GATHERER
During my ordeal, a number of my friends brought up the fact that I do not eat meat, which is a good source of B-12. The suggestion I think is that my wounds, on some level, were self-inflicted. It is true that vegans and vegetarians are more likely to be confronted with this problem. Having been a vegan myself for about a year in 2005 during my education as a chef, I respect their choice, even if it means committing to a regimen of B- 12 injections to avoid killing animals. I have opted for eating fish and organic eggs again, thanking the fish and chickens for their offerings. And I have upped my intake of sardines and salmon, which are two of the best B-12 sources, making peace with the fact that I am, like many other animals, a hunter, and gatherer.
 Editor’s Note: Dree Andrea is an international award-winning filmmaker, artist, and energy coach working in New York and New Jersey. Her B-12 journey has taken her in some fascinating directions and led her to some eye-opening studies on B-12 deficiency. There is research that suggests that her hypersensitivity may have been further amplified by the fact that her mother carried twins, but that her sibling died in the womb. She is currently enrolled in the only training that specializes in coaching highly sensitive people and empaths. Dree is working on her second book, The Empath and the Psychopath, and on the documentary Losing Your Marbles; A B-12 Side Effect. Dree can be found at dreeinthebigcity.com.
Editor’s Note: Dree Andrea is an international award-winning filmmaker, artist, and energy coach working in New York and New Jersey. Her B-12 journey has taken her in some fascinating directions and led her to some eye-opening studies on B-12 deficiency. There is research that suggests that her hypersensitivity may have been further amplified by the fact that her mother carried twins, but that her sibling died in the womb. She is currently enrolled in the only training that specializes in coaching highly sensitive people and empaths. Dree is working on her second book, The Empath and the Psychopath, and on the documentary Losing Your Marbles; A B-12 Side Effect. Dree can be found at dreeinthebigcity.com.




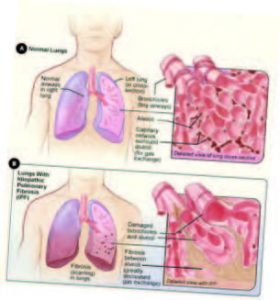
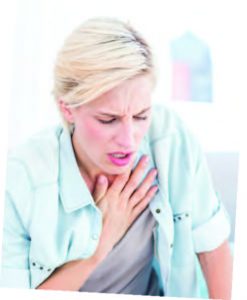
 In the summer of 2017, my mother lost her life to pulmonary fibrosis, the puzzling disease that takes your life by literally taking your breath. The illness plagued her through a 16-year-long battle that began in her 30s. She never saw it coming. She was at the height of her success when the disease crept into her life, robbing her of her dreams, her mobility and, ultimately, her time. I witnessed her excruciating decline and her diminished quality of life starting when I was in grade school. During those years, I wrestled with some difficult questions about the origin of the disease, its management and, of course, whether I too might be gasping for air one day.
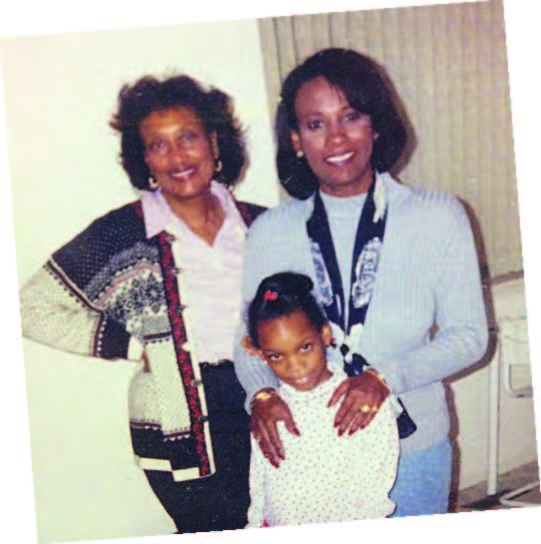
In the summer of 2017, my mother lost her life to pulmonary fibrosis, the puzzling disease that takes your life by literally taking your breath. The illness plagued her through a 16-year-long battle that began in her 30s. She never saw it coming. She was at the height of her success when the disease crept into her life, robbing her of her dreams, her mobility and, ultimately, her time. I witnessed her excruciating decline and her diminished quality of life starting when I was in grade school. During those years, I wrestled with some difficult questions about the origin of the disease, its management and, of course, whether I too might be gasping for air one day. You may be familiar with my mother’s work. Her name was Tracey Smith-Owens and she conducted celebrity interviews (as Tracey Smith) for EDGE until her passing. She had a knack for engaging people—including Louis Gossett, Chazz Palminteri and Frank Vincent—in thoughtful conversation, and often carried those conversations past the magazine’s pages into civilian life.
You may be familiar with my mother’s work. Her name was Tracey Smith-Owens and she conducted celebrity interviews (as Tracey Smith) for EDGE until her passing. She had a knack for engaging people—including Louis Gossett, Chazz Palminteri and Frank Vincent—in thoughtful conversation, and often carried those conversations past the magazine’s pages into civilian life. My mother was in the hospital for over a month until peacefully departing in her sleep. I never saw it coming; pulmonary fibrosis is full of surprises. My mother and her lungs were true fighters, the doctors told me. Her ability to survive and in many ways thrive for more than a decade-and-a-half astounded them.
My mother was in the hospital for over a month until peacefully departing in her sleep. I never saw it coming; pulmonary fibrosis is full of surprises. My mother and her lungs were true fighters, the doctors told me. Her ability to survive and in many ways thrive for more than a decade-and-a-half astounded them.




 If anyone can speak with authentic candor to a ballroom full of people about behavioral health and addiction, and make them simultaneously laugh out loud and nod in empathy, it’s Patrick J. Kennedy II, the former U.S. Congressman, mental health advocate and author of the New York Times Bestselling book titled A Common Struggle: A Personal Journey Through the Past and Future of Mental Illness and Addiction (Blue Rider Press, New York, 2016).
If anyone can speak with authentic candor to a ballroom full of people about behavioral health and addiction, and make them simultaneously laugh out loud and nod in empathy, it’s Patrick J. Kennedy II, the former U.S. Congressman, mental health advocate and author of the New York Times Bestselling book titled A Common Struggle: A Personal Journey Through the Past and Future of Mental Illness and Addiction (Blue Rider Press, New York, 2016). In October 2018, the Trinitas Health Foundation launched their Peace of Mind Campaign with an informative evening with Journalist Jack Ford moderating a conversation with Kennedy on “Easing the Stigma about Behavioral Health” at The Park Savoy Estate, Florham Park.
In October 2018, the Trinitas Health Foundation launched their Peace of Mind Campaign with an informative evening with Journalist Jack Ford moderating a conversation with Kennedy on “Easing the Stigma about Behavioral Health” at The Park Savoy Estate, Florham Park.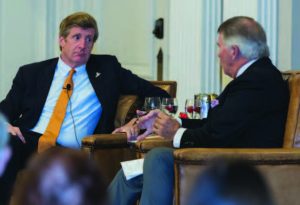 The event raised $235,000 toward the $4 million renovation project to update Trinitas’ Behavioral Health facility, one of the most comprehensive departments of behavioral health and psychiatry in New Jersey. They offer specialized services for adults, children and their families, as well as services for those with various addictions, and a 98-bed inpatient facility. The hospital welcomes nearly 200,000 behavioral health visits per year. The multi-disciplinary and bi-lingual staff includes psychiatrists, psychologists, social workers, nurses, creative arts therapists, substance abuse counselors and mental health workers, offering such services as psychiatric, emergency response/screening center, inpatient, outpatient, partial hospital programs and addiction services.
The event raised $235,000 toward the $4 million renovation project to update Trinitas’ Behavioral Health facility, one of the most comprehensive departments of behavioral health and psychiatry in New Jersey. They offer specialized services for adults, children and their families, as well as services for those with various addictions, and a 98-bed inpatient facility. The hospital welcomes nearly 200,000 behavioral health visits per year. The multi-disciplinary and bi-lingual staff includes psychiatrists, psychologists, social workers, nurses, creative arts therapists, substance abuse counselors and mental health workers, offering such services as psychiatric, emergency response/screening center, inpatient, outpatient, partial hospital programs and addiction services.


 LET THERE BE LIGHT
LET THERE BE LIGHT A SLUG’S LIFE
A SLUG’S LIFE EARLY ONSET DEMENTIA
EARLY ONSET DEMENTIA MOSAIC VACCINE
MOSAIC VACCINE SLOWING ALZHEIMER’S
SLOWING ALZHEIMER’S SPECIAL K
SPECIAL K EXPLOSIVE DEVELOPMENT
EXPLOSIVE DEVELOPMENT
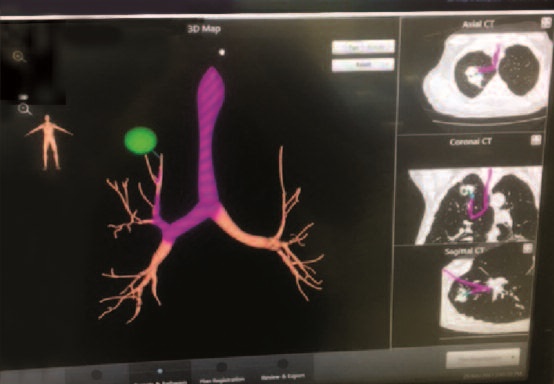 Where lung cancer is concerned, it is all about early detection. The 10-year survival rate for patients diagnosed in Stage 1 or 2 is 88 percent; in Stage 3 and 4, the five-year survival rate is just 17 percent. In his presentation, Dr. Remolina encouraged his fellow doctors to be more proactive when it comes to using the new technology. Medicare actually covers lung screening for “30-pack smokers” ages 55 and over, and Trinitas has a superb Lung Screening Program that employs a low-dose CT scan.
Where lung cancer is concerned, it is all about early detection. The 10-year survival rate for patients diagnosed in Stage 1 or 2 is 88 percent; in Stage 3 and 4, the five-year survival rate is just 17 percent. In his presentation, Dr. Remolina encouraged his fellow doctors to be more proactive when it comes to using the new technology. Medicare actually covers lung screening for “30-pack smokers” ages 55 and over, and Trinitas has a superb Lung Screening Program that employs a low-dose CT scan. Carlos Remolina, MD, FCCP, PA
Carlos Remolina, MD, FCCP, PA

 The year she was diagnosed, it had only been 11 months since her previous mammogram, which meant it would not be covered by insurance. She paid for it and that’s when it was discovered. “Had I waited and we went away for the summer like we usually did, it would have been another four months. My instincts were good
The year she was diagnosed, it had only been 11 months since her previous mammogram, which meant it would not be covered by insurance. She paid for it and that’s when it was discovered. “Had I waited and we went away for the summer like we usually did, it would have been another four months. My instincts were good She had a double mastectomy and chemotherapy, and shortly after being released from the hospital, her oldest daughter learned that she had a lump that needed to be removed. It was benign and she has been fine ever since
She had a double mastectomy and chemotherapy, and shortly after being released from the hospital, her oldest daughter learned that she had a lump that needed to be removed. It was benign and she has been fine ever since Just in time for Breast Cancer Awareness Month, the $3.4 million Connie Dwyer Breast Center opened at Trinitas on October 1 with a ribbon-cutting ceremony featuring Connie Dwyer, the Trinitas leadership, local officials such as Elizabeth Mayor Christian Bollwage, and a special guest appearance by Grammy award-winning singer Gloria Gaynor (left, with Connie), who sang “I Will Survive
Just in time for Breast Cancer Awareness Month, the $3.4 million Connie Dwyer Breast Center opened at Trinitas on October 1 with a ribbon-cutting ceremony featuring Connie Dwyer, the Trinitas leadership, local officials such as Elizabeth Mayor Christian Bollwage, and a special guest appearance by Grammy award-winning singer Gloria Gaynor (left, with Connie), who sang “I Will Survive The Breast Center, staffed with board-certified bilingual specialists, offers the most up-to-date equipment and services available, such as 3D imaging, which allows radiologists to view the breast tissue in several layers. This breakthrough technology can detect 41 percent more invasive breast
The Breast Center, staffed with board-certified bilingual specialists, offers the most up-to-date equipment and services available, such as 3D imaging, which allows radiologists to view the breast tissue in several layers. This breakthrough technology can detect 41 percent more invasive breast 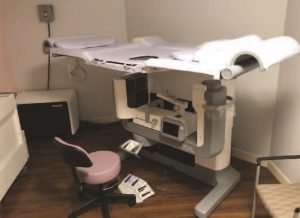


 A traumatic experience with the medical community early on in my life in Amsterdam (where I was born and raised) had motivated me to study a variety of holistic healing modalities after I came to America. When health issues arose that I could not address myself, I had worked successfully with a chiropractor and an acupuncturist, but never a traditional GP. Once, while experiencing severe pain after being clipped by a hit-and-run driver, a colleague convinced me to take an aspirin. It made me so sick that I decided to never touch over-the-counter medication again. Arnica gel for sprained ankles and Old Indian Wild Cherry bark for severe coughs were as far as I would go, no matter how grave the situation. I was a happy, healthy artist and documentary filmmaker living in the States for over 20 years when I began to “lose my mind.”
A traumatic experience with the medical community early on in my life in Amsterdam (where I was born and raised) had motivated me to study a variety of holistic healing modalities after I came to America. When health issues arose that I could not address myself, I had worked successfully with a chiropractor and an acupuncturist, but never a traditional GP. Once, while experiencing severe pain after being clipped by a hit-and-run driver, a colleague convinced me to take an aspirin. It made me so sick that I decided to never touch over-the-counter medication again. Arnica gel for sprained ankles and Old Indian Wild Cherry bark for severe coughs were as far as I would go, no matter how grave the situation. I was a happy, healthy artist and documentary filmmaker living in the States for over 20 years when I began to “lose my mind.”



 HUNTER GATHERER
HUNTER GATHERER Editor’s Note: Dree Andrea is an international award-winning filmmaker, artist, and energy coach working in New York and New Jersey. Her B-12 journey has taken her in some fascinating directions and led her to some eye-opening studies on B-12 deficiency. There is research that suggests that her hypersensitivity may have been further amplified by the fact that her mother carried twins, but that her sibling died in the womb. She is currently enrolled in the only training that specializes in coaching highly sensitive people and empaths. Dree is working on her second book, The Empath and the Psychopath, and on the documentary Losing Your Marbles; A B-12 Side Effect. Dree can be found at dreeinthebigcity.com.
Editor’s Note: Dree Andrea is an international award-winning filmmaker, artist, and energy coach working in New York and New Jersey. Her B-12 journey has taken her in some fascinating directions and led her to some eye-opening studies on B-12 deficiency. There is research that suggests that her hypersensitivity may have been further amplified by the fact that her mother carried twins, but that her sibling died in the womb. She is currently enrolled in the only training that specializes in coaching highly sensitive people and empaths. Dree is working on her second book, The Empath and the Psychopath, and on the documentary Losing Your Marbles; A B-12 Side Effect. Dree can be found at dreeinthebigcity.com.
 As the program began to take shape, The Haiti Student Nurse Project soon became known as Global Connections in Nursing Education: Haiti and the USA – a name that aptly communicates its essence: assuring that Haitian nurses have access to learning the best practices used in the US that they can then apply in responding to the needs of their fellow Haitians. Since 2014, the program has educated student nurses enrolled at Université de Notre Dame in Jacmel, Haiti, located about 100 miles south of Port au Prince. Its goal: to improve healthcare by strengthening the competence of its nurses. The student nurses have flown to New Jersey to undergo total immersion in US nursing practices and procedures, making the program one of the very few, if not the only one of its kind, to bring students to the United States for their learning experience.
As the program began to take shape, The Haiti Student Nurse Project soon became known as Global Connections in Nursing Education: Haiti and the USA – a name that aptly communicates its essence: assuring that Haitian nurses have access to learning the best practices used in the US that they can then apply in responding to the needs of their fellow Haitians. Since 2014, the program has educated student nurses enrolled at Université de Notre Dame in Jacmel, Haiti, located about 100 miles south of Port au Prince. Its goal: to improve healthcare by strengthening the competence of its nurses. The student nurses have flown to New Jersey to undergo total immersion in US nursing practices and procedures, making the program one of the very few, if not the only one of its kind, to bring students to the United States for their learning experience.

 FOCAL POINTS
FOCAL POINTS
 Cryotherapy is an ergonomic modality used to address a wide range of aches, pains and medical conditions. It also has benefits for athletes looking to improve their performance. The ancient Greeks and Romans used cryotherapy (immersion in chilly seawater) to treat inflamed wounds. In the 19th century, European medicine rediscovered this technique. A couple of generations ago, cryotherapy looked a lot different: a bag of ice wrapped around a knee or shoulder, a chilled whirlpool bath. In the 1970s, Japanese researcher Dr. Toshiba Yamauchi pioneered the concept of whole-body cryotherapy to treat rheumatoid arthritis and, in doing so, began to notice its therapeutic side effects for subjects who suffered from injuries and chronic inflammation. Since then, there has been a huge amount of medical information coming out about this technology and how it can benefit the human body in myriad ways.
Cryotherapy is an ergonomic modality used to address a wide range of aches, pains and medical conditions. It also has benefits for athletes looking to improve their performance. The ancient Greeks and Romans used cryotherapy (immersion in chilly seawater) to treat inflamed wounds. In the 19th century, European medicine rediscovered this technique. A couple of generations ago, cryotherapy looked a lot different: a bag of ice wrapped around a knee or shoulder, a chilled whirlpool bath. In the 1970s, Japanese researcher Dr. Toshiba Yamauchi pioneered the concept of whole-body cryotherapy to treat rheumatoid arthritis and, in doing so, began to notice its therapeutic side effects for subjects who suffered from injuries and chronic inflammation. Since then, there has been a huge amount of medical information coming out about this technology and how it can benefit the human body in myriad ways.


 By definition, the HFNJ’s mission is to improve the health and well-being of vulnerable, underserved populations in greater Newark and the Jewish Community of MetroWest NJ, to elevate the quality of community healthcare, reduce disparities in access, and promote the infusion of compassion and humanism into our healthcare system. Dr. Beth Levithan, chair of the HFNJ, who joined the board in 1997, is most proud of the HFNJ’s commitment to humanism.
By definition, the HFNJ’s mission is to improve the health and well-being of vulnerable, underserved populations in greater Newark and the Jewish Community of MetroWest NJ, to elevate the quality of community healthcare, reduce disparities in access, and promote the infusion of compassion and humanism into our healthcare system. Dr. Beth Levithan, chair of the HFNJ, who joined the board in 1997, is most proud of the HFNJ’s commitment to humanism.









 What is it about tears that make them such fertile territory for songwriters? Think, for instance, about how many times you’ve heard the words Don’t Cry as song lyrics: The Four Seasons (“Big Girls Don’t Cry”), Melissa Manchester (“Don’t Cry Out Loud”), Guns n Roses (“Don’t Cry”) and of course the signature song from Evita (“Don’t Cry for Me, Argentina”). The irony is that the inability to produce healthy tears can be a sign of a serious medical situation. Indeed, keratoconjunctivitis sicca—better known as Dry Eye Syndrome—affects millions of people each year. Based on data derived from the 2013 National Health & Wellness Survey, the percentage of Americans with dry eye could be as high as 6.8 percent—and the number of cases promises to increase steadily in the near future.
What is it about tears that make them such fertile territory for songwriters? Think, for instance, about how many times you’ve heard the words Don’t Cry as song lyrics: The Four Seasons (“Big Girls Don’t Cry”), Melissa Manchester (“Don’t Cry Out Loud”), Guns n Roses (“Don’t Cry”) and of course the signature song from Evita (“Don’t Cry for Me, Argentina”). The irony is that the inability to produce healthy tears can be a sign of a serious medical situation. Indeed, keratoconjunctivitis sicca—better known as Dry Eye Syndrome—affects millions of people each year. Based on data derived from the 2013 National Health & Wellness Survey, the percentage of Americans with dry eye could be as high as 6.8 percent—and the number of cases promises to increase steadily in the near future. What’s the secret to good eye health? Dr. Confino recommends balancing good nutrition with getting enough rest and also treating the eye as if it were a muscle—“that is, exercising it and caring for it with the same respect as any large muscle in the body.”
What’s the secret to good eye health? Dr. Confino recommends balancing good nutrition with getting enough rest and also treating the eye as if it were a muscle—“that is, exercising it and caring for it with the same respect as any large muscle in the body.”  Joel Confino’s specialty is cataract surgery. He is a graduate of the Albert Einstein College of Medicine and completed his Ophthalmology residency at Mount Sinai School of Medicine.
Joel Confino’s specialty is cataract surgery. He is a graduate of the Albert Einstein College of Medicine and completed his Ophthalmology residency at Mount Sinai School of Medicine.  Erica O’Lenick is a graduate of the Pennsylvania College of Optometry. She has experience in pediatric, binocular vision care, ocular disease, and anterior segment care.
Erica O’Lenick is a graduate of the Pennsylvania College of Optometry. She has experience in pediatric, binocular vision care, ocular disease, and anterior segment care.
 According to the American Sleep Association (ASA), nearly one in 10 adults in this country suffers from sleep apnea. Around half have a snoring problem. Two in five adults fall asleep during the day when they should be awake, with an alarmingly high 5% reporting that they do so while driving at least once a month. The ASA also attributes between 3% and 5% of obesity to sleep deprivation. Not surprisingly, insomnia tops the chart of sleep issues.
According to the American Sleep Association (ASA), nearly one in 10 adults in this country suffers from sleep apnea. Around half have a snoring problem. Two in five adults fall asleep during the day when they should be awake, with an alarmingly high 5% reporting that they do so while driving at least once a month. The ASA also attributes between 3% and 5% of obesity to sleep deprivation. Not surprisingly, insomnia tops the chart of sleep issues. The Sleep Disorders Center is equipped with all state-of-the-art diagnostic equipment to monitor heart, breathing and muscle activity, as well as specialized equipment such as the BiPAP machine, a non-invasive form of therapy for patients suffering from sleep apnea. Videos are an important tool in sleep analysis and are regularly reviewed with patients to help them understand the source of their sleeplessness.
The Sleep Disorders Center is equipped with all state-of-the-art diagnostic equipment to monitor heart, breathing and muscle activity, as well as specialized equipment such as the BiPAP machine, a non-invasive form of therapy for patients suffering from sleep apnea. Videos are an important tool in sleep analysis and are regularly reviewed with patients to help them understand the source of their sleeplessness.






 Dr. Pidkaminetskiy is especially impressed with the community-oriented approach of the practice, as well as the convenience of close contact with his colleagues to expedite immediate consultations and sharing of vital patient information. Patients similarly appreciate the wide range of medical services and treatments provided by Trinitas and the ease with which care can be both delivered and accessed at the various practice offices.
Dr. Pidkaminetskiy is especially impressed with the community-oriented approach of the practice, as well as the convenience of close contact with his colleagues to expedite immediate consultations and sharing of vital patient information. Patients similarly appreciate the wide range of medical services and treatments provided by Trinitas and the ease with which care can be both delivered and accessed at the various practice offices. Jazmyn Thomas (pictured right), a current patient of the Medical Group, appreciated Dr. Baerga’s kindness before, during, and after having minor surgery. “He was very supportive,” said the Elizabeth resident. “I called him with questions every day, sometimes more than once, and he never made me feel like I was a bother. Even when he wasn’t in the office, he managed to get back to me right away. He made me feel a lot better about everything, especially because I had never had surgery before.”
Jazmyn Thomas (pictured right), a current patient of the Medical Group, appreciated Dr. Baerga’s kindness before, during, and after having minor surgery. “He was very supportive,” said the Elizabeth resident. “I called him with questions every day, sometimes more than once, and he never made me feel like I was a bother. Even when he wasn’t in the office, he managed to get back to me right away. He made me feel a lot better about everything, especially because I had never had surgery before.”
 The Trinitas Medical Group offers a large and growing staff of
The Trinitas Medical Group offers a large and growing staff of 


 Adam Rowen, MD
Adam Rowen, MD





 THE TEAM
THE TEAM
 Crunch Time
Crunch Time 
 Into the Woods
Into the Woods 
 Cervical Cancer’s “Racial Divide”
Cervical Cancer’s “Racial Divide”  But Is It An Organ?
But Is It An Organ?  Real-Time Concussion Detector
Real-Time Concussion Detector 
 Early Detection for Autism
Early Detection for Autism 


 Though born and raised in Minnesota, Dr. Perrone is no stranger to the Garden State. He made his first New Jersey connection in college, graduating from Rutgers and receiving his medical degree from the University of Medicine and Dentistry of New Jersey (UMDNJ). He completed his residency at the Mayo Clinic School of Graduate Medical Education and has been practicing obstetrical gynecology for 21 years. He led his own private practice in Rochester, Minnesota as part of Olmstead Medical Center, a not-for-profit organization serving southern Minnesota.
Though born and raised in Minnesota, Dr. Perrone is no stranger to the Garden State. He made his first New Jersey connection in college, graduating from Rutgers and receiving his medical degree from the University of Medicine and Dentistry of New Jersey (UMDNJ). He completed his residency at the Mayo Clinic School of Graduate Medical Education and has been practicing obstetrical gynecology for 21 years. He led his own private practice in Rochester, Minnesota as part of Olmstead Medical Center, a not-for-profit organization serving southern Minnesota. 

 GH: I was in my 11th year as a CEO at Our Lady of Mercy in the Bronx. Trinitas was a challenge—and I always look for a challenge. I was at an age where, if I was going to make a change, I had to make it, and I was in the prime of my administrative background. I was very impressed with the committee evaluating the candidates, and the Board of Trustees, I had an opportunity to meet the administrative staff and I was impressed with the organization and the merger. However, I knew there were challenges in the culture of one hospital against another hospital. Looking back, we have done things that frankly, in my own mind, I didn’t think we’d be able to accomplish. One of the biggest difficulties was becoming financially stable as a newly merged institution, which can create a lot of chaos. We had to reduce the staff and evaluate the organizational leadership as to whether the chemistry was right between all the different executives. I’m pleased that the changes we made have been long-standing. Most of the people I’ve brought in have been here with me almost as long as I have.
GH: I was in my 11th year as a CEO at Our Lady of Mercy in the Bronx. Trinitas was a challenge—and I always look for a challenge. I was at an age where, if I was going to make a change, I had to make it, and I was in the prime of my administrative background. I was very impressed with the committee evaluating the candidates, and the Board of Trustees, I had an opportunity to meet the administrative staff and I was impressed with the organization and the merger. However, I knew there were challenges in the culture of one hospital against another hospital. Looking back, we have done things that frankly, in my own mind, I didn’t think we’d be able to accomplish. One of the biggest difficulties was becoming financially stable as a newly merged institution, which can create a lot of chaos. We had to reduce the staff and evaluate the organizational leadership as to whether the chemistry was right between all the different executives. I’m pleased that the changes we made have been long-standing. Most of the people I’ve brought in have been here with me almost as long as I have.