If shingles “doesn’t care,” should you take that personally?

www.istockphoto.com
If you watch any amount of cable news or network television, you’re probably under the impression that shingles is more than a disease. It’s an inevitability. After all, anyone who’s had chicken pox as a kid already has the virus, right? Scarier still is the seeming randomness of shingles: “Almost one in three people will develop shingles in their lifetime.” Who is this person? Who are the other two? And is there some indicator or precondition or lifestyle choice that tilts the odds against me?
These are all reasonable questions your healthcare provider can answer on your next visit. Until then, here are a few facts to mull over.
According to the CDC, that “almost one-in-three” statistic is accurate. Older adults are far more likely to develop shingles than young adults, and shingles in children is extremely unusual. The hot-poker/electric-shock special effect in the commercials is not an overstatement of the nerve pain some people experience at the site of the shingles rash—its technical name is postherpetic neuralgia (PHN)—but fewer than 20% of shingles sufferers actually experience PHN. For most, it’s about the itch.
Although shingles is usually a one-and-done condition, it is possible to have a recurrence. Also, really bad cases can lead to hospitalization. According to the CDC that number is between 1 and 4%, and is usually a combination of old age and a suppressed or compromised immune system. Rates of shingles cases among older Americans have remained steady for 15 years, but have increased somewhat among younger adults. No on one is certain why that is.
In most cases, shingles presents as a band-like rash on one side of the body, or on the face. You’re likely to get a warning sign, such as an itch or tingling in the area where the rash is about to occur. The rash itself blisters and then scabs over and clears up in less than a month. During that time, shingles sufferers may experience fever or headaches and nausea.

www.istockphoto.com
Shingles respond to a number of antiviral medicines, which shorten the length and severity of the illness. The sooner treatment begins, the more effective it tends to be. Even when the pain is mild, the itch can drive you a bit mad, so doctors will typically suggest wet compresses, oatmeal baths and old reliable calamine lotion. Certain foods should also be avoided during an outbreak, including dark chocolate and soy products, which contain the amino acid Arginine. Most doctors will advise you to pump the brakes on caffeine and alcohol during recovery.
If you develop shingles, or know someone who has, rest assured that shingles cannot be directly transmitted. However, those who have never been vaccinated for chicken pox, or never had it, can develop chicken pox after coming into contact with fluid from shingles blisters.
In almost all cases, as the commercials say, the virus has been in your body since childhood (especially if you were born in the 1970s or earlier). The chicken pox virus, varicella zoster (VZV), can stay dormant in the human nervous system for decades and then suddenly reactivate.
Shingrix, the recombinant zoster vaccine (RZV) is recommended by the CDC for people over 50 and for younger adults whose immune systems have been weakened by disease or therapy.
“Adults 50 years and older should get two doses of Shingrix, separated by two to six months,” says Dr. Muniba Naqi, an internal medicine specialist at Trinitas. “Younger adults 19 years and older who have—or will have—weakened immune systems should also get two doses of Shingrix. Diseases that weaken the immune system include chronic inflammatory conditions such as lupus and rheumatoid arthritis, or any underlying malignancy, as well as HIV and transplant patients.”

www.istockphoto.com
Shingrix has proven to be more than 90% effective in preventing shingles and PHN, and provides strong immunity for at least seven years. It replaces Zostavax, an older vaccine that was far less effective.
“Some people will develop shingles despite vaccination,” cautions Dr. Naqi. “However, the vaccine may reduce its severity and duration. It can also reduce the risk of postherpetic neuralgia, the shingles complication that causes pain to continue long after the blisters have cleared.”
So who gets shingles and who doesn’t? First off, you don’t “catch” shingles. The best answer, unfortunately, is the vaguest. VZV appears to have the highest chance of reactivating when your immune system isn’t functioning at 100%.
As we age, it becomes increasingly difficult to maintain a high-functioning immune system, which is why the older you get, the more likely you are to be one of the “nearly one in three” that develops shingles. Other contributors can include heavy use of anti-inflammatory medications, as well as the immune-suppressing meds associated with Crohn’s disease, lupus and rheumatoid arthritis—which are in line with the disease Dr. Naqi lists.
Finally, there’s our old friend, stress. Stress can do a number on your immune system, sometimes without your even knowing it. Not only can it open the door enough to reactivate VZV, it can also make the symptoms of shingles much worse once you have it.
 Editor’s Note:
Editor’s Note:
Dr. Muniba Naqi is an internal medicine specialist and Medical Director of Hospitalist Medicine at Trinitas. Dr. Naqi has been the founding Medical Director for the Trinitas Hospitalist Department for the past seven years.










 I think of myself as an adventurous person and I have done more traveling than most—to Southeast Asia twice, several countries in Europe, and Mexico several times. I am comfortable interacting with people and respectful of their cultures. I had never been to Africa, however, and was not familiar with Tanzania before I arrived. I was unsure what to expect, although I knew that the hospital where I would be working was not going to be comparable to anything we have here in the United States.
I think of myself as an adventurous person and I have done more traveling than most—to Southeast Asia twice, several countries in Europe, and Mexico several times. I am comfortable interacting with people and respectful of their cultures. I had never been to Africa, however, and was not familiar with Tanzania before I arrived. I was unsure what to expect, although I knew that the hospital where I would be working was not going to be comparable to anything we have here in the United States.

 The first time I was in the delivery room at Trinitas, I really felt like I was part of a team. It all seemed very natural to me. The baby was born after a long, 24-hour labor. It was striking how much work the mother did, how exhausted she was, and how miserable she was while going through the most physically difficult thing she’ll probably do in her life—and then seeing that “switch” when she was holding her baby for the first time and how all that suddenly didn’t matter. She was happy and glowing and crying. And I was crying.
The first time I was in the delivery room at Trinitas, I really felt like I was part of a team. It all seemed very natural to me. The baby was born after a long, 24-hour labor. It was striking how much work the mother did, how exhausted she was, and how miserable she was while going through the most physically difficult thing she’ll probably do in her life—and then seeing that “switch” when she was holding her baby for the first time and how all that suddenly didn’t matter. She was happy and glowing and crying. And I was crying. Along with the learning opportunity came certain challenges for which it turned out I was unprepared. Resources we take for granted here are scarce to non-existent. For example, we had one fetal heartrate monitor for the whole floor, no IV pumps, and there were no individual rooms for the patients. Each area was divided into bays by plastic curtains. In each bay was a bed, a stool and an empty nightstand. Patients brought their own supplies to the hospitals—including sheets, pillows and drinking water. The only thing provided was a basic Foley catheter. The different wards in the hospital were connected by outdoor walkways. There were few if any doors separating inside from outside, including in the surgical ward.
Along with the learning opportunity came certain challenges for which it turned out I was unprepared. Resources we take for granted here are scarce to non-existent. For example, we had one fetal heartrate monitor for the whole floor, no IV pumps, and there were no individual rooms for the patients. Each area was divided into bays by plastic curtains. In each bay was a bed, a stool and an empty nightstand. Patients brought their own supplies to the hospitals—including sheets, pillows and drinking water. The only thing provided was a basic Foley catheter. The different wards in the hospital were connected by outdoor walkways. There were few if any doors separating inside from outside, including in the surgical ward. In Tanzania, I gained tremendous confidence being put in situations that I had only learned about in a lecture. During my time at Muhimbili University National Hospital, I was able to apply absolutely everything I learned at the Trinitas School of Nursing to my patients in Tanzania—and I know that everything I learned in Dar es Salaam I will bring into my future nursing practice.
In Tanzania, I gained tremendous confidence being put in situations that I had only learned about in a lecture. During my time at Muhimbili University National Hospital, I was able to apply absolutely everything I learned at the Trinitas School of Nursing to my patients in Tanzania—and I know that everything I learned in Dar es Salaam I will bring into my future nursing practice. Editor’s Note: Alexandra Redmond will be taking her boards early this year and hopes to be working in a neonatal intensive care unit (NICU) in 2023.
Editor’s Note: Alexandra Redmond will be taking her boards early this year and hopes to be working in a neonatal intensive care unit (NICU) in 2023.




 Editor’s Note: Dr. Muniba Naqi is an internal medicine specialist and Medical Director of Hospitalist Medicine at Trinitas. Dr. Naqi has been the founding Medical Director for the Trinitas Hospitalist Department for the past seven years.
Editor’s Note: Dr. Muniba Naqi is an internal medicine specialist and Medical Director of Hospitalist Medicine at Trinitas. Dr. Naqi has been the founding Medical Director for the Trinitas Hospitalist Department for the past seven years.


 rehabilitation nurses, Judy Christianson and Jean Mikita. They all consider Antonetta a major success story and hosted a 90th birthday celebration for her this summer. “I enjoy the time I spend at the Center,” Antonetta says. “I look forward to it and it helps me get my day started. Jean, Judy and Hugh tease me a bit about how I’m a ‘flirt’ but they just like to bring a smile to my face.”
rehabilitation nurses, Judy Christianson and Jean Mikita. They all consider Antonetta a major success story and hosted a 90th birthday celebration for her this summer. “I enjoy the time I spend at the Center,” Antonetta says. “I look forward to it and it helps me get my day started. Jean, Judy and Hugh tease me a bit about how I’m a ‘flirt’ but they just like to bring a smile to my face.”
 Trinitas Regional Medical Center, Dr. Ari S. Eckman, M.D., sees a steady stream of patients dealing with diabetes—a disease approaching epidemic proportions— and also hypothyroidism, another disorder that is growing, particularly among women. When asked if his high-risk patients were better dieters than most, the Chief of TRMC’s Division of Endocrinology, Diabetes & Metabolism said that yes, initially they are. “But many do lapse over time,” he admits. Apparently, risk alone is no guarantee of success. Dr. Eckman is quick to confirm this fact. He maintains that dieting is not so much about food as it is about lifestyle. The root of the word “diet” actually comes from the Greek word diaita, which means a “prescribed way of living.” Dieting, he insists, doesn’t have to mean depriving. That being said, he cautions, the whole point of dieting is to lose weight. “Make no mistake about that.” The Power of Positive Eating Google “diet” on your computer and the results are overwhelming. You’ll discover page after page of sites that are overflowing with imaginative menus and mouthwatering recipes. Whichever one you choose, says Dr. Eckman, you can increase the chance for success by following these ground rules: Spice Up Your Life Although salt can amp up flavor, there are a lot of other herbs and spices, both dried and fresh, that can compensate: pepper, oregano, basil, cumin, garlic, cilantro and the well-sung quartet of parsley, sage, rosemary, and thyme.
Trinitas Regional Medical Center, Dr. Ari S. Eckman, M.D., sees a steady stream of patients dealing with diabetes—a disease approaching epidemic proportions— and also hypothyroidism, another disorder that is growing, particularly among women. When asked if his high-risk patients were better dieters than most, the Chief of TRMC’s Division of Endocrinology, Diabetes & Metabolism said that yes, initially they are. “But many do lapse over time,” he admits. Apparently, risk alone is no guarantee of success. Dr. Eckman is quick to confirm this fact. He maintains that dieting is not so much about food as it is about lifestyle. The root of the word “diet” actually comes from the Greek word diaita, which means a “prescribed way of living.” Dieting, he insists, doesn’t have to mean depriving. That being said, he cautions, the whole point of dieting is to lose weight. “Make no mistake about that.” The Power of Positive Eating Google “diet” on your computer and the results are overwhelming. You’ll discover page after page of sites that are overflowing with imaginative menus and mouthwatering recipes. Whichever one you choose, says Dr. Eckman, you can increase the chance for success by following these ground rules: Spice Up Your Life Although salt can amp up flavor, there are a lot of other herbs and spices, both dried and fresh, that can compensate: pepper, oregano, basil, cumin, garlic, cilantro and the well-sung quartet of parsley, sage, rosemary, and thyme. Most Americans need to reduce their daily salt intake. This is doubly true for people trying to lose weight. Think Outside the Box Get creative in your kitchen. Take advantage of seasonal produce. Cook veggies several different ways (roast, steam, grill) for different taste and texture…and raw is always beautiful. Make fruit a part of your meal to stave off a major sugar craving. Dress Up Your Diet Visually feast, don’t just blindly eat! Set a pretty plate. Garnish your heart out. Color-coordinate healthy food choices. Use your best china. Sip water out of a crystal goblet. Presentation goes a long way—cater to all of your senses, not just your taste buds. Move Away from the Kitchen At home, dine someplace other than where the food is, namely the kitchen. You’ll have to get up for second helpings. The extra steps will make you take notice of how much you’re consuming. Work In a Workout A diet without exercise is a recipe for failure. Find 30 minutes each day to break a sweat with some cardio activity, and not necessarily all in a single interval. Park your car a little farther from the office or the supermarket. If you work at home, devote the commuting time saved to exercise. No buts to getting off your butt. Lead Yourself Not into Temptation Drive by the driveins. Clean out your cupboards. Eat five to six small meals a day rather than only two; your body seeks to metabolize— deny it by skipping a meal and you’ll overeat at the next. Monitor the Usual Suspects Forego the fad diets; better to identify your specific food weaknesses and just stay away from them. That way a minor slip-up won’t lead to a major binge! Among the same search-engine results that yield great recipes for different diets, you will also find lengthy dissertations on the challenges to success: temptation, boredom, stress, self-indulgence and the need for instant gratification. To that, says Dr. Eckman, you can add resentment. Nothing can sabotage a diet’s success more than hating the fact that you have to diet at all. Ultimately, he says, we will comfort ourselves by giving in to cravings. We’ll indulge ourselves with dangerous “treats.” We’ll eat, drink and yet we still won’t feel particularly merry. Denial is also a definite diet-killer, adds Dr. Eckman. “Too often I hear patients claim that they don’t eat much! The problem is how much is ‘much’ to them? And it may not even be how much they eat, but how wrong they eat,” he says. “If you can’t see the real you when you look in the mirror, then maybe you need to go out and buy a good scale…and then be sure to step on it.” The numbers won’t lie. EDGE
Most Americans need to reduce their daily salt intake. This is doubly true for people trying to lose weight. Think Outside the Box Get creative in your kitchen. Take advantage of seasonal produce. Cook veggies several different ways (roast, steam, grill) for different taste and texture…and raw is always beautiful. Make fruit a part of your meal to stave off a major sugar craving. Dress Up Your Diet Visually feast, don’t just blindly eat! Set a pretty plate. Garnish your heart out. Color-coordinate healthy food choices. Use your best china. Sip water out of a crystal goblet. Presentation goes a long way—cater to all of your senses, not just your taste buds. Move Away from the Kitchen At home, dine someplace other than where the food is, namely the kitchen. You’ll have to get up for second helpings. The extra steps will make you take notice of how much you’re consuming. Work In a Workout A diet without exercise is a recipe for failure. Find 30 minutes each day to break a sweat with some cardio activity, and not necessarily all in a single interval. Park your car a little farther from the office or the supermarket. If you work at home, devote the commuting time saved to exercise. No buts to getting off your butt. Lead Yourself Not into Temptation Drive by the driveins. Clean out your cupboards. Eat five to six small meals a day rather than only two; your body seeks to metabolize— deny it by skipping a meal and you’ll overeat at the next. Monitor the Usual Suspects Forego the fad diets; better to identify your specific food weaknesses and just stay away from them. That way a minor slip-up won’t lead to a major binge! Among the same search-engine results that yield great recipes for different diets, you will also find lengthy dissertations on the challenges to success: temptation, boredom, stress, self-indulgence and the need for instant gratification. To that, says Dr. Eckman, you can add resentment. Nothing can sabotage a diet’s success more than hating the fact that you have to diet at all. Ultimately, he says, we will comfort ourselves by giving in to cravings. We’ll indulge ourselves with dangerous “treats.” We’ll eat, drink and yet we still won’t feel particularly merry. Denial is also a definite diet-killer, adds Dr. Eckman. “Too often I hear patients claim that they don’t eat much! The problem is how much is ‘much’ to them? And it may not even be how much they eat, but how wrong they eat,” he says. “If you can’t see the real you when you look in the mirror, then maybe you need to go out and buy a good scale…and then be sure to step on it.” The numbers won’t lie. EDGE 
 trying to get healthy food into a picky eater. If the kid is yours, however, it’s no joke. There are reasons for your child’s peculiar eating habits, and things you can do to broaden his or her culinary horizons. First off, you may be surprised to learn that it’s hardly ever a matter of taste. Picky eating is a natural part of toddlerhood, as children express their independence. What parents may believe is a fussy eater may not actually be that at all. “Children don’t tend to eat as much at meals as adults expect them to eat, and babies spit out their food, leading parents to believe that they don’t like it,” says Dr. Maria Padron, a pediatric and adolescent psychiatrist at Trinitas Regional Medical Center. “But babies taste food by spitting it out and licki
trying to get healthy food into a picky eater. If the kid is yours, however, it’s no joke. There are reasons for your child’s peculiar eating habits, and things you can do to broaden his or her culinary horizons. First off, you may be surprised to learn that it’s hardly ever a matter of taste. Picky eating is a natural part of toddlerhood, as children express their independence. What parents may believe is a fussy eater may not actually be that at all. “Children don’t tend to eat as much at meals as adults expect them to eat, and babies spit out their food, leading parents to believe that they don’t like it,” says Dr. Maria Padron, a pediatric and adolescent psychiatrist at Trinitas Regional Medical Center. “But babies taste food by spitting it out and licki ng it, and if parents believe their child doesn’t like it and don’t continue to introduce that food, it becomes a foreign food to them.” Well-meaning parents may try to cater to a picky eater, but experts say that that only backfires. “They create a monster,” Dr. Padron explains. “Unless there’s a medical contraindication, children should be ‘helped’ to eat everything that the family eats.” Easier said than done, right? Don’t give up until you’ve exhausted these strategies: Offer variety earlier. “Kids often become picky eaters because they haven’t been exposed to a lot of foods,” Dr. Padron says. “You should slowly expose children to different kinds of foods.” Hold your ground. Your child may decide to go on a hunger strike for a meal or two if you suddenly stop being a short order cook and insist that he eats what you’re eating, but he won’t hold out forever. “Kids may refuse to eat for a few meals, but as long as they’re healthy and still drinking liquids, it’s fine,” Dr. Padron says. “When he’s hungry, your child will eat.” Keep reintroducing the same food. “Parents need to be patient w
ng it, and if parents believe their child doesn’t like it and don’t continue to introduce that food, it becomes a foreign food to them.” Well-meaning parents may try to cater to a picky eater, but experts say that that only backfires. “They create a monster,” Dr. Padron explains. “Unless there’s a medical contraindication, children should be ‘helped’ to eat everything that the family eats.” Easier said than done, right? Don’t give up until you’ve exhausted these strategies: Offer variety earlier. “Kids often become picky eaters because they haven’t been exposed to a lot of foods,” Dr. Padron says. “You should slowly expose children to different kinds of foods.” Hold your ground. Your child may decide to go on a hunger strike for a meal or two if you suddenly stop being a short order cook and insist that he eats what you’re eating, but he won’t hold out forever. “Kids may refuse to eat for a few meals, but as long as they’re healthy and still drinking liquids, it’s fine,” Dr. Padron says. “When he’s hungry, your child will eat.” Keep reintroducing the same food. “Parents need to be patient w hen they’re introducing new foods, and not get upset if kids aren’t jumping to eat broccoli right away,” Dr. Padron advises. Even if your children didn’t like asparagus the first few times, all it may take is the repetition (or a new way of serving it) to make them like it the 10th time around. You just need to insist on one bite each time you serve it— if they still don’t like it, don’t force it. Get your kids involved. Take your kids along to the grocery store and let them choose something new to try in the produce department—and if you have the time, let them get involved in preparing the dinner, too. By allowing your child to have a say in what they’re eating and an investment in the meal, you may find that they’re more willing to eat the fruit they picked out or the side dish they helped make. Minimize distractions at dinnertime. If there are other forms of entertainment beyond eating—a TV, books or toys—that can keep kids from attending to the task at hand. Instead, look for ways to make the meal itself more entertaining, with a colorful variety of vegetables or interesting presentations. Seek help. Get your pediatrician on board, especially if it’s been a long-standing issue, where your child’s eating habits may have become ingrained. For more severe cases, your pediatrician may recommend speaking to an expert, such as a counselor or a speech or occupational therapist. Indeed, in some instances, picky eating can be the sign of a more serious issue—a sensory disorder or a mechanical issue with feeding. So when is the right time to call in professional help? “In children with feeding issues, it could be a textural or tactile issue, often with mushy foods like bananas or yogurt,” says Kevin Nelson, occupational therapist and Manager of Trinitas Children’s Therapy Services. “Or it can be a mechanical issue, where they simply don’t have the musculature in their mouth to handle that food.” Whatever the cause of a child’s pickiness, in the end the key is to work slowly. Your kid won’t become an adventurous eater overnight, and if the issues are more sensory or mechanical in nature, you may need to follow a much gentler, slower path toward introducing these foods.
hen they’re introducing new foods, and not get upset if kids aren’t jumping to eat broccoli right away,” Dr. Padron advises. Even if your children didn’t like asparagus the first few times, all it may take is the repetition (or a new way of serving it) to make them like it the 10th time around. You just need to insist on one bite each time you serve it— if they still don’t like it, don’t force it. Get your kids involved. Take your kids along to the grocery store and let them choose something new to try in the produce department—and if you have the time, let them get involved in preparing the dinner, too. By allowing your child to have a say in what they’re eating and an investment in the meal, you may find that they’re more willing to eat the fruit they picked out or the side dish they helped make. Minimize distractions at dinnertime. If there are other forms of entertainment beyond eating—a TV, books or toys—that can keep kids from attending to the task at hand. Instead, look for ways to make the meal itself more entertaining, with a colorful variety of vegetables or interesting presentations. Seek help. Get your pediatrician on board, especially if it’s been a long-standing issue, where your child’s eating habits may have become ingrained. For more severe cases, your pediatrician may recommend speaking to an expert, such as a counselor or a speech or occupational therapist. Indeed, in some instances, picky eating can be the sign of a more serious issue—a sensory disorder or a mechanical issue with feeding. So when is the right time to call in professional help? “In children with feeding issues, it could be a textural or tactile issue, often with mushy foods like bananas or yogurt,” says Kevin Nelson, occupational therapist and Manager of Trinitas Children’s Therapy Services. “Or it can be a mechanical issue, where they simply don’t have the musculature in their mouth to handle that food.” Whatever the cause of a child’s pickiness, in the end the key is to work slowly. Your kid won’t become an adventurous eater overnight, and if the issues are more sensory or mechanical in nature, you may need to follow a much gentler, slower path toward introducing these foods.

 The casualty list in this epic, microscopic battle being waged within your body includes a runny nose, scratchy throat, watery eyes, itchy hives and, in the most serious cases, a potentially lifethreatening asthma attack. “Pet dander can activate cells in the immune system,” confirms Samuel D. Kahnowitz, MD, FCCP, FACP, Chief of Pulmonary Medicine and Medical Director of Respiratory Therapy at Trinitas Regional Medical Center. “The body then makes inflammatory substances that constrict the muscles around the airway, and cause swelling on the inside of the airways, making it harder to breathe.” Reactions to pet allergies account for an increasing number of doctor and emergency room visits in this country, so the medical community is taking this trend seriously. To a layman, at least, the obvious question is, “Has pet dander somehow gotten ‘worse’ or are people becoming more sensitive to it?” Actually the same question could be asked about our food and environment—allergies in general seem to be more prevalent, and more serious, than ever. It turns out that we may be the problem. Indeed studies suggest that our country’s obsession with cleanliness may be to blame for creating hypersensitive immune systems, which now react to harmless things around us. “Our environment has improved, so we don’t have to worry about fighting off dangerous parasites,” explains Richard J. Bukosky, MD, an allergist in Linden. “The allergic antibody doesn’t have a whole lot to do. It starts to ‘pick’ on things that we’re exposed to in the environment that are completely harmless.” While there is still no permanent cure for pet allergies, there are plenty of options available for minimizing their effects on your life—and many of them don’t require finding a new home for Fluffy or Fido: Minimize exposure to pets. The less exposure to the offending pet, the better. Opting to find a new home for your pet may help in the long run, though it can take up to 20 weeks after the pet leaves before the allergen levels really dissipate.
The casualty list in this epic, microscopic battle being waged within your body includes a runny nose, scratchy throat, watery eyes, itchy hives and, in the most serious cases, a potentially lifethreatening asthma attack. “Pet dander can activate cells in the immune system,” confirms Samuel D. Kahnowitz, MD, FCCP, FACP, Chief of Pulmonary Medicine and Medical Director of Respiratory Therapy at Trinitas Regional Medical Center. “The body then makes inflammatory substances that constrict the muscles around the airway, and cause swelling on the inside of the airways, making it harder to breathe.” Reactions to pet allergies account for an increasing number of doctor and emergency room visits in this country, so the medical community is taking this trend seriously. To a layman, at least, the obvious question is, “Has pet dander somehow gotten ‘worse’ or are people becoming more sensitive to it?” Actually the same question could be asked about our food and environment—allergies in general seem to be more prevalent, and more serious, than ever. It turns out that we may be the problem. Indeed studies suggest that our country’s obsession with cleanliness may be to blame for creating hypersensitive immune systems, which now react to harmless things around us. “Our environment has improved, so we don’t have to worry about fighting off dangerous parasites,” explains Richard J. Bukosky, MD, an allergist in Linden. “The allergic antibody doesn’t have a whole lot to do. It starts to ‘pick’ on things that we’re exposed to in the environment that are completely harmless.” While there is still no permanent cure for pet allergies, there are plenty of options available for minimizing their effects on your life—and many of them don’t require finding a new home for Fluffy or Fido: Minimize exposure to pets. The less exposure to the offending pet, the better. Opting to find a new home for your pet may help in the long run, though it can take up to 20 weeks after the pet leaves before the allergen levels really dissipate.  If your dog or cat is here to stay, make sure to keep it out of your bedroom—the place where you spend most of your time—and wash your hands thoroughly after you’ve touched your pet. Weekly bathing or grooming (done by someone other than the person with the allergies) may also help keep allergens at bay. Keep it clean. Daily vacuuming and washing-down of surfaces can help clear some of the allergens—especially if you use a vacuum with a HEPA filter that can trap the tiny particles. Removing carpeting, drapery, stuffed toys and other soft fabrics can help reduce the number of places where pet dander can become trapped. “I really push for them to allergy-proof the bedroom—get rid of the carpeting and the animals, get a dehumidifier and a HEPA filter, avoid down comforters and get allergy-proofing casing for the pillows and mattresses,” Dr. Bukosky says. Consider that it might not be your pet. Even if allergy testing turns up an allergic reaction, it may not actually be your animal that’s causing the wheezing. “Dogs roam around, and it might not be the dog himself—it may be an irritant he’s picking up outside, like wood chips or rag weed,” says Dr. Kahnowitz. Take antihistamines. Newer over-the-counter formulations, like Zyrtec and Claritin, are more potent and less likely to cause drowsiness and other unpleasant side effects. Try a more serious approach. Doctors have become more aggressive in treating allergies, often including steroids in the treatment plan. “We’re pushing steroids more,” Dr. Bukosky says. “We used to use a montelukast (Singulair) a lot, but we’ve started to use inhaled steroids more—for nasal allergies, internasal steroids are a good option.” Of course, pet allergies can also be treated with a program of allergy immunizations. “We push for immunizations, which make it less likely that you’ll develop asthma,” says Dr. Bukosky. The regimens generally start with weekly shots, then as the treatment progresses, patients can go longer and longer between injections. Finally, there’s the do-nothing approach. These are the people who claim they have built an immunity to their animal. Is this really possible? The answer is yes…and no. Dr. Bukosky warns that what these pet owners believe to be happening may not actually be the case. “With daily exposure to the pet, a person with allergies may be having mild allergy-like attacks each day that use up the IgE antibody—just not enough to cause symptoms,” he says. “Then the child goes off to college, or is away from the pet for a long vacation, and has an asthma attack. So you may become ‘used to’ your pet, but you have to be in constant contact with it to avoid a serious reaction.”
If your dog or cat is here to stay, make sure to keep it out of your bedroom—the place where you spend most of your time—and wash your hands thoroughly after you’ve touched your pet. Weekly bathing or grooming (done by someone other than the person with the allergies) may also help keep allergens at bay. Keep it clean. Daily vacuuming and washing-down of surfaces can help clear some of the allergens—especially if you use a vacuum with a HEPA filter that can trap the tiny particles. Removing carpeting, drapery, stuffed toys and other soft fabrics can help reduce the number of places where pet dander can become trapped. “I really push for them to allergy-proof the bedroom—get rid of the carpeting and the animals, get a dehumidifier and a HEPA filter, avoid down comforters and get allergy-proofing casing for the pillows and mattresses,” Dr. Bukosky says. Consider that it might not be your pet. Even if allergy testing turns up an allergic reaction, it may not actually be your animal that’s causing the wheezing. “Dogs roam around, and it might not be the dog himself—it may be an irritant he’s picking up outside, like wood chips or rag weed,” says Dr. Kahnowitz. Take antihistamines. Newer over-the-counter formulations, like Zyrtec and Claritin, are more potent and less likely to cause drowsiness and other unpleasant side effects. Try a more serious approach. Doctors have become more aggressive in treating allergies, often including steroids in the treatment plan. “We’re pushing steroids more,” Dr. Bukosky says. “We used to use a montelukast (Singulair) a lot, but we’ve started to use inhaled steroids more—for nasal allergies, internasal steroids are a good option.” Of course, pet allergies can also be treated with a program of allergy immunizations. “We push for immunizations, which make it less likely that you’ll develop asthma,” says Dr. Bukosky. The regimens generally start with weekly shots, then as the treatment progresses, patients can go longer and longer between injections. Finally, there’s the do-nothing approach. These are the people who claim they have built an immunity to their animal. Is this really possible? The answer is yes…and no. Dr. Bukosky warns that what these pet owners believe to be happening may not actually be the case. “With daily exposure to the pet, a person with allergies may be having mild allergy-like attacks each day that use up the IgE antibody—just not enough to cause symptoms,” he says. “Then the child goes off to college, or is away from the pet for a long vacation, and has an asthma attack. So you may become ‘used to’ your pet, but you have to be in constant contact with it to avoid a serious reaction.”
 Heart attack victims who have pets tend to live longer. Watching fish in a tank can lower blood pressure. In senior adults, canine companionship can keep mental health complications from turning into physical deterioration. Indeed, considerable evidence supports the healing potential of pet therapy. There is plenty of history to back up the power of pet therapy, too. The first documented account of animal therapy dates back to the 9th century in Gheel, Belgium, where farm animals were used to help disabled people cope. In Washington, D.C. in 1919, psychiatric patients at St. Elizabeth’s Hospital had dogs available for their recognized therapeutic value. And in the decades since, the medical community has come to embrace this interactive approach to improving the quality of life, both for patients in recovery and for those whose health may be in decline. For the record, today the more politically correct term for pet-related therapy is either Animal-Assisted Activities (AAA) or Animal-Assisted Therapy (AAT). AAA is a more casual meet-and-greet approach to hands-on contact between patients and pets, while AAT is a more formal clinical approach with patients who may be challenged physically, emotionally, or mentally.
Heart attack victims who have pets tend to live longer. Watching fish in a tank can lower blood pressure. In senior adults, canine companionship can keep mental health complications from turning into physical deterioration. Indeed, considerable evidence supports the healing potential of pet therapy. There is plenty of history to back up the power of pet therapy, too. The first documented account of animal therapy dates back to the 9th century in Gheel, Belgium, where farm animals were used to help disabled people cope. In Washington, D.C. in 1919, psychiatric patients at St. Elizabeth’s Hospital had dogs available for their recognized therapeutic value. And in the decades since, the medical community has come to embrace this interactive approach to improving the quality of life, both for patients in recovery and for those whose health may be in decline. For the record, today the more politically correct term for pet-related therapy is either Animal-Assisted Activities (AAA) or Animal-Assisted Therapy (AAT). AAA is a more casual meet-and-greet approach to hands-on contact between patients and pets, while AAT is a more formal clinical approach with patients who may be challenged physically, emotionally, or mentally. her five-year old beagle, Murphy. Both have been certified by St. Hubert’s. Reynolds recognized early on that Murphy had the necessary qualifications, since he had become an ambassador of goodwill in her own neighborhood, particularly among senior residents. Currently, the psych department’s group sessions are held at Trinitas, with special visits paid to the on-site nursing facility—the domain of Harley, another gifted pet “therapist.” The adult outpatient groups are often organized according to particular challenge. Two of the currently active groups are focusing on anxiety relief and partial vs. unconditional love. Reynolds refers to these sessions as her “puppy love” groups. “I really just knew I had to share him,” Reynolds says of Murphy, who wears a hospital staff photo ID badge, as do all the therapy dogs. It is attached to his favorite bandana; Reynolds realized that Murphy needed a work wardrobe and provided it. Murphy is typically on the job two or three days a month. A typical day includes sessions with two to three groups, each with five to ten patients. Patients are not the only recipients of Murphy’s healing powers. Staff members having a bad day often drop by for a visit and a pet. Murphy is happy to oblige. “No stranger is too strange for Murphy,” Reynolds says.
her five-year old beagle, Murphy. Both have been certified by St. Hubert’s. Reynolds recognized early on that Murphy had the necessary qualifications, since he had become an ambassador of goodwill in her own neighborhood, particularly among senior residents. Currently, the psych department’s group sessions are held at Trinitas, with special visits paid to the on-site nursing facility—the domain of Harley, another gifted pet “therapist.” The adult outpatient groups are often organized according to particular challenge. Two of the currently active groups are focusing on anxiety relief and partial vs. unconditional love. Reynolds refers to these sessions as her “puppy love” groups. “I really just knew I had to share him,” Reynolds says of Murphy, who wears a hospital staff photo ID badge, as do all the therapy dogs. It is attached to his favorite bandana; Reynolds realized that Murphy needed a work wardrobe and provided it. Murphy is typically on the job two or three days a month. A typical day includes sessions with two to three groups, each with five to ten patients. Patients are not the only recipients of Murphy’s healing powers. Staff members having a bad day often drop by for a visit and a pet. Murphy is happy to oblige. “No stranger is too strange for Murphy,” Reynolds says.






 “All of my life, I have watched my family do charitable work,” she explains. “My grandfather was a physician, my mother was a physician, and through them doing their jobs, I felt like this was a career I wanted to pursue—where I could actually go out into the community to help people and gain personal satisfaction from contributing to medical society.”
“All of my life, I have watched my family do charitable work,” she explains. “My grandfather was a physician, my mother was a physician, and through them doing their jobs, I felt like this was a career I wanted to pursue—where I could actually go out into the community to help people and gain personal satisfaction from contributing to medical society.”
 Movers & (Salt) Shakers
Movers & (Salt) Shakers
 Bum Deal for New Yorkers
Bum Deal for New Yorkers
 $150 Up in Smoke
$150 Up in Smoke Nothing Rotten in the State of Denmark
Nothing Rotten in the State of Denmark
 Link Between Heartburn & Heart Attacks
Link Between Heartburn & Heart Attacks CBT Helping Insomniacs Hit the Snooze Button
CBT Helping Insomniacs Hit the Snooze Button


 They Do More Than Play Football at LSU
They Do More Than Play Football at LSU The Five-Second Rule: A Second Look
The Five-Second Rule: A Second Look Surprising Findings in Oral Cancer Study
Surprising Findings in Oral Cancer Study
 Home Games
Home Games
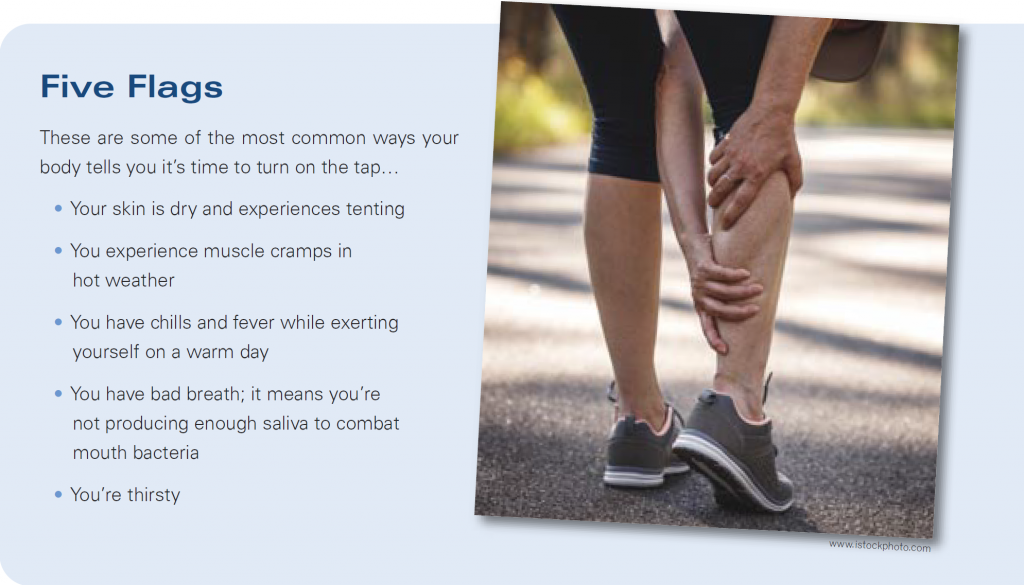
 Number One Not So Fun
Number One Not So Fun



 Editors Note: Chris Gibbs pulled this assignment because she has a long history with carpal tunnel syndrome. In other words, it’s personal. Is the computer, she asked, the culprit in the rise in cases? Dr. Mackessy says the jury is still out on that connection. The same goes for texting and thumb issues. Instead he is convinced that almost everyone will suffer from some degree of rotator cuff or carpal or other hand damage once they reach a certain age—through the normal wear and tear of everyday life.
Editors Note: Chris Gibbs pulled this assignment because she has a long history with carpal tunnel syndrome. In other words, it’s personal. Is the computer, she asked, the culprit in the rise in cases? Dr. Mackessy says the jury is still out on that connection. The same goes for texting and thumb issues. Instead he is convinced that almost everyone will suffer from some degree of rotator cuff or carpal or other hand damage once they reach a certain age—through the normal wear and tear of everyday life.